“The average number of children U.S. adults think is ideal is 2.7. To achieve this family size, a sexually active woman must use contraceptives for roughly three decades.”
So reads a 2021 fact sheet on contraceptive use from the Guttmacher Institute, Planned Parenthood’s former research arm.
Three decades of contraceptive use is a long time. It’s a long time to expose oneself to the increased risks of both breast and cervical cancers (and, yes, while oral contraceptive use is associated with decreased risk of uterine, ovarian, and colorectal cancer, you can read more about why that doesn’t “balance out” the increased breast and cervical cancer risk, here). Likewise, three decades is a long time to negatively impact bone mineral density, especially given that a woman’s bone mineral density should be peaking during her teens and twenties. And it’s a devastating length of time to face increased risks for blood clots and an array of autoimmune disorders and mental health issues.
On the other side of the coin, thirty years is also a long time to miss out on the benefits of ovulation, a process which only occurs in healthy, naturally cycling women, as birth control functions primarily by preventing ovulation from happening. And ovulation is more than about the release of an egg each month–it is essential for female bone, breast, brain, heart, and immune health. Because women are often told by their doctors that birth control will “regulate” their cycles, many have no idea that they have no cycle on the Pill, and that the hormone withdrawal bleed they experience each month isn’t the same thing as a period. Here, I’ll cover the key hormonal difference between your natural cycle and your “cycle” on the Pill.
This is what happens to your hormones during a natural ovulatory cycle
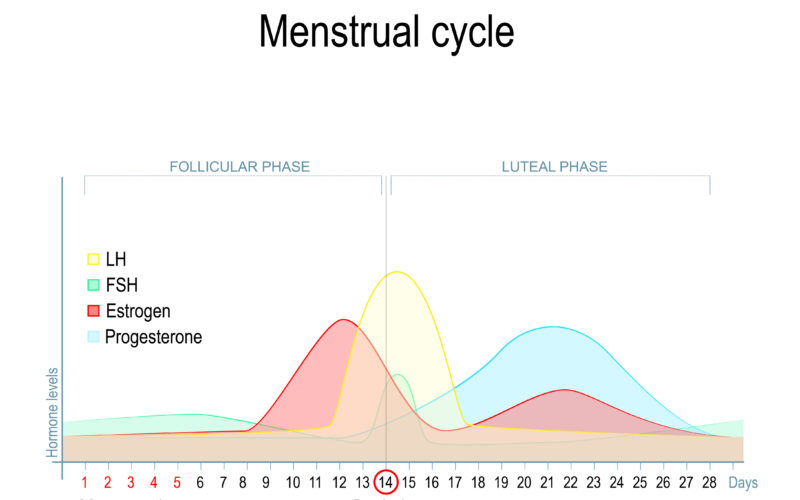
Follicular phase
In the first part of the cycle, we have the follicular phase (sometimes known as the proliferative phase), which starts towards the end of a woman’s menstrual period. During this phase, follicle stimulating hormone (FSH) levels increase in a woman’s brain, sending a message to one of her ovaries to recruit follicles (the structures surrounding each egg) to mature. The recruited follicles in the ovary start to grow and produce estrogen. A woman using a fertility awareness method (FAM) has evidence of this increase in estrogen levels when she notices a change in sensation from dryness to moisture at the vaginal opening (that feeling of moisture is actually due to the presence of cervical mucus, which you can read about more, here).
The selected follicles continue to produce more and more estrogen, which in turn causes the endometrial lining to thicken and causes the cervix to open (just a little bit!) and secrete a “sperm friendly” estrogenic, fertile mucus discharge. This is usually observed by the woman as a change in sensation from moist to slippery at the opening of the vagina.
The rapid rise of estrogen levels, along with small increases in progesterone and inhibin, signals the brain to decrease FSH. Peak estrogen levels typically produce an observable discharge around the time of ovulation that is clear and thin, like raw egg white (which is why other NW articles refer to this as egg-white cervical mucus, or EWCM). One follicle becomes “dominant” in this hormonal environment. This is the follicle that will release the egg at ovulation (aka the main event of your cycle).
Ovulation
Kisspeptin and Luteinizing hormone (LH)
Rapidly rising estrogen levels activate the hormone Kisspeptin in the brain (more on Kisspeptin and the surprising origin of its name, here!). The Kisspeptinergic system is influenced by many different hormones, and is necessary for the onset of puberty and for reproductive function. Activation of Kisspeptin by the rapid rise in estrogen levels causes the brain to release a surge of luteinizing hormone (LH), which is necessary to trigger ovulation. The released egg survives 12-24 hours if not fertilized, at which point it will break down and be resorbed by the woman’s body.
Corpus luteum
At the same time as the LH surge, the follicle secretes progesterone to maintain LH levels, allowing for the formation of the corpus luteum (or “yellow body,” which is covered at length, here). This rise in progesterone just before ovulation is very important for the health of the corpus luteum.
Luteal phase
The corpus luteum secretes progesterone (the dominant hormone during this phase of the cycle) and some estrogen to maintain an adequate luteal phase length. At this point, the thickening of the uterine lining (the endometrium) slows down, and increased progesterone enriches it with blood vessels and nutrients in preparation for possible implantation of a fertilized egg (embryo).
The mucus discharge secreted by the cervix changes from slippery and clear (estrogenic and fertile) to dry and thick (progestagenic and infertile) after ovulation. This blocks sperm from swimming through the cervix, acting as a biological valve. The corpus luteum lives 11 to 16 days (on average, 14) if the egg is not fertilized, and begins to shrink after about 6 days.
Menses / Your period
As the corpus luteum dissolves, about 14 days after ovulation, estrogen and progesterone levels drop, triggering the beginning of a new cycle with the sloughing of the endometrium. This is observed as vaginal bleeding or a “period.”
Menstrual bleeding is an important external indicator of how balanced the prior cycle’s hormones were, and how healthy the ovulation was. Of note: the cyclical bleeding that occurs while taking the Pill is a result of hormone withdrawal, not ovulation. Oral contraceptive pills (OCPs) stop ovulation by suppressing the hormonal communication between the brain and the ovaries [1].
Gonadotropin releasing hormone: the hormone that makes your entire cycle happen
Remember how I mentioned the “kisspeptinergic system” above? A healthy kisspeptinergic system in the brain supports Gonadotropin releasing Hormone (GnRH) function, and GnRH makes the whole hormonal process from the beginning of the follicular phase to the end of the follicular cycle happen. No GnRH means no menstruation, follicular phase, ovulation, or luteal phase.
GnRH is produced by the hypothalamus in the brain, and is released in a pattern of continuous, pulsating waves that change in amplitude depending on where you are in your cycle. This continuous pulsating release allows for the necessary hormonal fluctuations required to achieve ovulation. Quite the intricate system, no?
This is what happens to your hormones on the Pill (or any other form of hormonal contraception)
With the exception of the copper IUD and some progestin-only pills (sometimes called “mini Pills,”) all forms of contraception contain a combination of synthetic estrogens and progestins. The Pill (and other forms of hormonal contraception) works in 3 main ways to “flatline” your hormone levels (which we’ll discuss below), which stops your natural cycle altogether. That’s right: if you are on hormonal birth control, you do not have a cycle.
#1 Preventing ovulation by blocking the HPO feedback loop
The Pill’s primary mechanism of action for preventing conception is preventing ovulation by blocking the communication pathway of hormones between the brain and the ovaries. This “pathway” is known scientifically as the hypothalamic-pituitary-ovarian (HPO) feedback loop. This lowers the body’s natural estrogen and progesterone, to levels below which ovulation cannot occur. Concerningly, research suggests that women who have been on the Pill have lower blood levels of naturally occurring estrogen and progesterone, even after stopping the medication, than women who aren’t on hormonal contraception [2].
Dr. Juan Pablo Del Rio and colleagues’ description of the “ovulatory continuum” provides a compelling visual of this medically-induced hormonal imbalance. You can think of the normal hormonal variance observed in healthy, natural, ovulatory cycles as being like a normal cardiac rhythm electrocardiogram (EKG) tracing, with the up and down representing the “lub-dub” of a heartbeat. As you can see below, the Pill induces a “flatline” for FSH, LH, estrogen and progesterone. See Figure 1. from Del Rio et. al. [3].
#2 Thickening and drying up cervical mucus by blocking the effects of your body’s estrogen
The Pill also prevents conception by thickening and drying up cervical mucus. The synthetic progesterone (progestin) in the Pill counteracts the effects of the body’s natural estrogen, preventing the production of the slippery mucus (also known as “egg-white” mucus) necessary for sperm survival. Sperm survives only minutes to hours in a thickened mucus environment, and thickened mucus likewise forms a barrier that prevents sperm from ever reaching the mature egg (should the Pill’s primary mechanism of action fail, and ovulation still occur–a phenomenon known as breakthrough ovulation). The increased risk of cervical cancer associated with the Pill is attributed to this action [4].
#3 Thinning the uterine lining (endometrium) by suppressing the body’s own natural estrogen and progesterone
The third way the Pill works to prevent pregnancy* is by thinning the endometrium. The Pill prevents the thickening of the uterine lining that naturally occurs before ovulation, as well as the nourishment provided by the corpus luteum after ovulation.
In other words, the Pill is designed to keep the endometrium thin and flat, under 7 millimeters, typically between 2.5mm and 5.7 mm. The normal thickness of an endometrium after ovulation is 9-12mm, increasing to up to 16mm before shedding as one’s period. Optimum endometrial thickness associated with live births in patients undergoing in-vitro fertilization (IVF) was between 8.7 and 14.5mm [5]. This effect also explains the lighter bleeding and the decreased risk of endometrial cancer associated with the Pill.
Your “cycle” on the Pill isn’t a cycle at all
When you’re on the Pill or another form of hormonal contraception, your natural cycle is paused altogether (except for when breakthrough ovulation occasionally occurs), tricking your body not into “thinking it’s already pregnant,” as you may have heard, but into thinking it’s already ovulated. But because your body hasn’t actually ovulated while on the Pill, you miss out on the health benefits of ovulation and incur multiple health risks at the same time.
Fortunately, fertility awareness methods (FAM) offer women ways to prevent pregnancy, plan families, and address reproductive health issues that maintain, support, and even restore the body’s natural hormonal patterns and fertility health. Women’s bodies were incredibly designed, and FAMs respect that design rather than overriding the system as hormonal birth control does. Side effects need not apply. Best of all, FAMs and methods of Natural Family Planning (NFP) are just as effective as many of the most common contraceptives available on the market (don’t believe it? Read more on FAM effectiveness, here.)
*Note that we specified that the endometrial-thinning action of the Pill does not function to prevent conception, but pregnancy (which is defined as beginning only when an embryo implants within the endometrium). Should the primary and secondary mechanisms of action fail to prevent conception (prevention of ovulation and thickening of cervical mucus, respectively), this tertiary mechanism is intended to prevent implantation of the newly conceived embryo.
References:
[1] Westhoff CL, Heartwell S, Edwards S, Zieman M, et al. Oral contraceptive discontinuation: do side effects matter? Am J Obstet Gynecol. 2007 Apr;196(4):412.e1-6; discussion 412.e6-7. doi: 10.1016/j.ajog.2006.12.015. PMID: 17403440; PMCID: PMC1903378. [2] Fleischman, D. S., Navarrete, C. D., & Fessler, D. M. T. (2010). Oral Contraceptives Suppress Ovarian Hormone Production. Psychological Science, 21(5), 750–752. https://doi.org/10.1177/0956797610368062. [3] Del Río JP, Alliende M I, Molina N, et al. “Steroid Hormones and Their Action in Women’s Brains: The Importance of Hormonal Balance.” Front. Public Health, vol. 6 (2018). https://doi.org/10.3389/fpubh.2018.00141 [4] Guven, Suleyman et al. “The underlying cause of cervical cancer in oral contraceptive users may be related to cervical mucus changes.” Medical hypotheses vol. 69,3 (2007): 550-2. doi:10.1016/j.mehy.2007.01.051. [5] Shaodi, Zhang et al. “The effect of endometrial thickness on pregnancy outcomes of frozen-thawed embryo transfer cycles which underwent hormone replacement therapy.” PloS one vol. 15,9 e0239120. 24 Sep. 2020, doi:10.1371/journal.pone.0239120.Additional Reading:
FAM Basics: What is the luteal phase of the menstrual cycle?
FAM Basics: What is the follicular phase of the menstrual cycle?