When you hear the term “reproductive organs” you are most likely to think about the parts on the lower half of your body. But the mammary glands in breast tissue are an essential reproductive organ as well. Breast tissue development happens in 3 distinct phases: first in the womb, second during puberty, and third during pregnancy and lactation. While we will cover all three of these developmental phases in this article, the second phase (the pubertal phase) in particular provides us with yet another important biological reason why women need their periods.
Additionally, since breast cancer is the second leading cause of death in women in the U.S., we’ll also cover whether having your period increases your breast cancer risk–plus one surefire way to decrease your breast cancer risk.
Breast development occurs during 3 necessary phases
Phase 1: Breast development from conception through 2 years of age
As early as 4-6 weeks gestation, a female fetus has cells that will lead to the development of her breast. Throughout the entire pregnancy, the mammary glands of a female fetus grow and develop by creating a system of thin tubes or ducts in the breast that will carry milk from the breast lobules to the nipple.
By the fifth month of gestation, the nipple on each breast has been created. After birth and up until 2 years of age, breast tissue grows by branching and forming lobes, sections in the breast that will eventually produce milk. After 2 years of age, breast tissue remains dormant until puberty.
Phase 2: Breast development during puberty
The sex hormones estrogen and progesterone don’t just direct the events of each menstrual cycle, they also directly impact breast tissue. During puberty, outward, visible signs of breast development can be seen, as estrogen (produced via ovulation, as girls begin to cycle) causes adipose (fatty) tissue to begin collecting, leading to enlargement of the breasts.
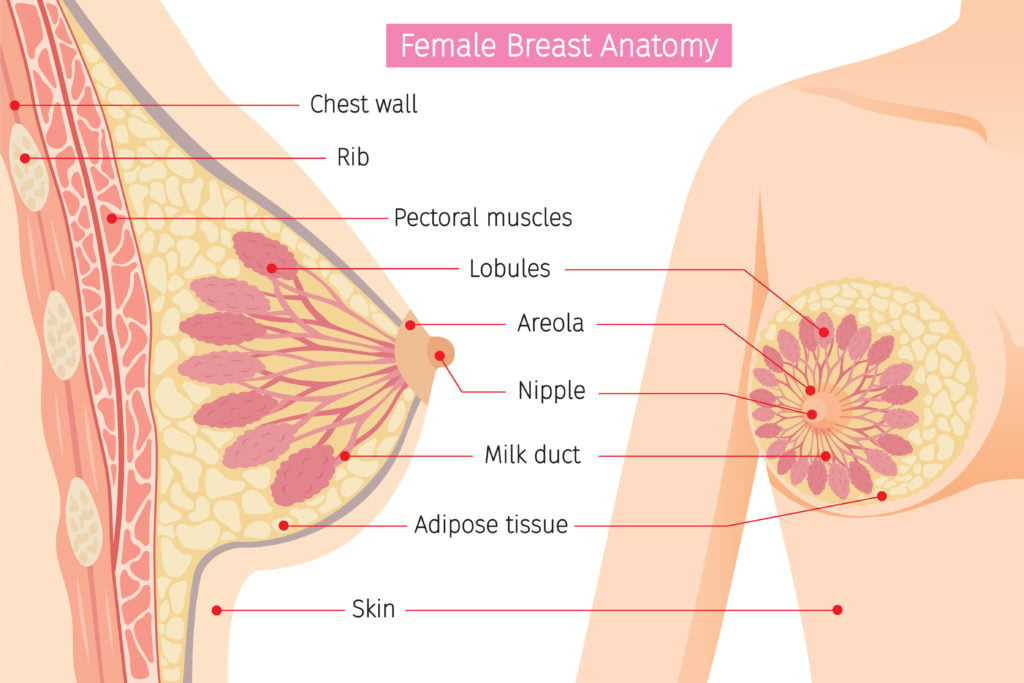
But breast tissue composition is not just fatty tissue, although that is an important part of it. Breast tissue also includes the system that produces and transports the milk to the nipple: lobes, lobules, milk ducts, and fibrous connective tissue. There are usually anywhere from 15 to 24 lobes, or sections, in each breast, and tiny lobules inside the lobes produce milk.
The most critical reason a natural cycle matters for a young woman’s future ability to breastfeed is that during each menstrual cycle, more milk ducts are produced. Estrogen and progesterone are thought to be responsible for ductal elongation and side branching, respectively. Internally, as breast tissue is undergoing this second phase of development, the ductal system continues to grow and develop and the glands that will produce milk begin to form at the end of the milk ducts. This process will continue throughout puberty, as ovulation and menstruation begin in earnest.
It is particularly common for teens to feel tingling, tenderness, and sensitivity in their breast tissue both during ovulation and approaching menstruation. This is due to the peak levels of estrogen mid-cycle, and the withdrawal of progesterone that occurs before menstruation.
However, young girls who take hormonal contraceptives are deprived of their menstrual cycles, and thus the cyclic exposure to the very endogenous hormones needed for proper branching and growth of the milk ducts. Additionally, teens who experience untreated hormone cycle disturbances like the irregular cycles common in polycystic ovary syndrome (PCOS) may also miss out on proper breast development.
Phase 3: Breast development during pregnancy and lactation
The final stage of maturation of breast tissue begins during pregnancy as early as 4 weeks gestation, right about the time one might see a positive on an at-home early pregnancy test. Tenderness, discomfort, and tingling in the breasts are all normal symptoms of this stage. Many pregnant women notice more veins visible externally on the breast, darker areolas, and may even experience the leaking of colostrum as early as the second trimester.
As we explained in depth here, cancer-vulnerable Type 1 and Type 2 lobules mature to cancer-resistant Type 3 and Type 4 lobules during this final stage of breast development, more specifically, around 32 weeks gestation. Mammary glands continue to develop and prepare for lactation right up until the expulsion of the placenta after childbirth, which triggers full-on milk production.
This is yet another reason why the menstrual cycle is so important for breast health: one has to ovulate regularly (and well) to be able to get pregnant, and experiencing a full-term pregnancy is known to be protective against breast cancer.
Is menstruation connected to breast cancer risk?
But you may have heard that how long and how often you menstruate is connected to breast cancer risk, such that the more times you menstruate, the higher your risk for breast cancer may be [1]. This connection might seem odd because women have menstruated since the dawn of time, and yet breast cancer rates have skyrocketed in the last century. Why might this be?
Several Swedish researchers first began to study “menstrual cycle length, menstrual regularity, and the number of menstrual cycles as risk factors for breast cancer” back in the 1990s [2]. In 2020, they published a summary of the results of research done since their early studies. In a table format, they showed that 13 studies “indicate that a high number of cycles before the first full-term pregnancy and high life-time menstrual activity (LMA) increased breast cancer risk. Furthermore, a short time interval between menarche [first period] and the establishment of regular cycles is another risk factor” [2].
While the researchers believed that “cyclic hormonal stimulation of the breast tissue [aka during the menstrual cycle]… is probably the most important hormonal factor contributing to breast cancer,” they acknowledged that it “is not directly investigated” in the existing research (emphasis added) [2]. They wrote that long-term prospective studies, in which women are followed over the course of a lifetime, are needed to better understand the connection between menstruation and breast cancer risk since, to date, studies have primarily asked women to recall when they had their first period and other menstrual cycle characteristics retrospectively, meaning long after the fact.
The researchers also noted that studies have often used “average measures of menstrual factors,” meaning that the fluctuations in things like cycle length that women normally experience over the course of their reproductive lifespan aren’t taken into account [2]. The researchers specifically state that “Development of better methods to describe the menstrual cycle more exact (sic) is needed” and they actually mention tracking cervical mucus or basal body temperature as ways to do this [2]!
We see from the above that more research in this area is needed. But it stands to reason that because a woman’s breast tissue matures to be more cancer-resistant towards the end of her first full-term pregnancy, the longer a woman cycles before her first full term pregnancy, then, the more cancer-vulnerable she would logically be. It also makes sense that having your first full-term pregnancy at a younger age (versus at an older age) would be more protective against breast cancer.
Here’s how you can definitely decrease your breast cancer risk
While there’s much we don’t fully understand yet about the connection between menstruation and breast cancer risk, lactation has a definitively protective effect against breast cancer development, particularly for those women who breastfeed for more than a year, both by reducing exposure to estrogen by delaying the return of ovulation, and by shedding breast tissue that could contain damaged or mutated DNA, according to cancer experts at MD Anderson.
Women who are most likely to lactate or breastfeed for a year (or longer) tend to be women who have supportive practitioners, workplaces, and family members. They also tend to have been exposed to proper breast tissue development for optimum milk production. That means breast tissue development happened properly during the 3 stages from gestation, to puberty, to pregnancy.
In contrast, suppression of cycles (read: lack of menstruation and ovulation) in the teen years may negatively affect lactation down the road, even if pregnancy occurs more than a decade later. Simply put, a teenager on hormonal contraception isn’t exposed to the hormones responsible for dramatically increasing the number and elongation of milk ducts. Consequently, it is possible that women who took hormonal birth control in their teen years could go on to have fewer milk ducts than they would have developed otherwise–which might mean difficulty with breastfeeding down the road, leading to lesser duration of breastfeeding, and less of a protective effect against breast cancer.
As we’ve seen above and in our related pieces on bone, immune, heart, and brain health, women, need to have their periods! Far from being just a regular inconvenience, or only relevant in regards to a woman’s desire to achieve or prevent pregnancy, the menstrual cycle matters for every woman’s overall health. Breast health is yet another important piece in the overall big picture of why women need periods.
References:
[1] Collaborative Group on Hormonal Factors in Breast Cancer. Menarche, menopause, and breast cancer risk: individual participant meta-analysis, including 118 964 women with breast cancer from 117 epidemiological studies. The Lancet Oncology. 2012; 13:1141-1151. doi.org/10.1016/S1470-2045(12)70425-4 [2] Olsson HL, Olsson ML. The Menstrual Cycle and Risk of Breast Cancer: A Review. Front Oncol. 2020;10:21. Published 2020 Jan 24. doi:10.3389/fonc.2020.00021 [3] Brisken C, et al. A paracrine role for the epithelial progesterone receptor in mammary gland development. Proc Natl Acad Sci U S A. 1998 Apr 28;95(9):5076-81. doi: 10.1073/pnas.95.9.5076. PMID: 9560231; PMCID: PMC20216.Additional Reading:
How birth control, pregnancy, and abortion each impact a woman’s breast cancer risk
As breastfeeding rates soar, the WHO doubles down on promoting birth control
Who cares about breast cancer?
Does birth control prevent-or cause- breast cancer?
Reasons women need periods: the role of the menstrual cycle in heart health
Reasons women need periods: the role of the menstrual cycle in bone health and development








What about a daughter who has shown signs of puberty but still no period by age 16?