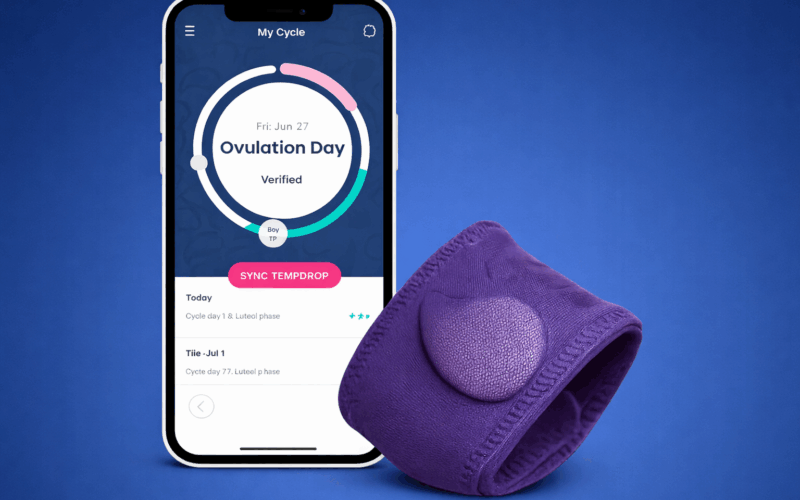
A 2025 research study of 194 cycles from 125 women found that the Tempdrop wearable thermometer, which continuously measures axillary (armpit) temperature while the wearer sleeps, identified ovulation comparably to ClearBlue urinary hormone ovulation tests [1]. Additionally, Tempdrop data now syncs with the Apple Health app.
This is promising news both for women seeking to use basal body temperature readings for pregnancy avoidance or achievement, as well as for women seeking additional biodata for personal health and wellness, particularly the millions of women who use the Apple Health app.
The science behind basal body temperature (BBT) for fertility tracking
Basal body temperature (BBT, which I previously covered in-depth here) is your body’s lowest resting temperature in a 24-hour period, which occurs while you’re sleeping. The post-ovulation temperature rise (first documented in 1905 by the Dutch gynecologist Theodoor Hendrik van de Velde) is a consequence of elevated progesterone levels, which are driven by the corpus luteum [2]. This is one of multiple ways the body prepares for a potential pregnancy, and another reminder of how a healthy menstrual cycle, as observed by biomarkers, signals that all is well with the body!
As one Tempdrop review mentioned, some women may even see their BBT decrease just slightly about 1-2 days before ovulation, followed by a rise of between 0.4 and 1 degree after ovulation. The BBT should then remain elevated until your period starts, when it returns to pre-ovulatory levels. (In the case of a pregnancy, the BBT remains elevated.)
Why you can’t track basal body temperature with a standard thermometer
The relatively small temperature shift after ovulation is the reason you need a basal body thermometer, which measures to hundredths of a degree, or two decimal places, rather than to tenths of a degree, or one decimal place, as standard drugstore oral thermometers do.
Using BBT to achieve or avoid pregnancy
For decades, women have utilized BBT monitoring alongside cervical mucus observations (and optional cervical position observations) as part of the symptothermal method of natural family planning, to either achieve or avoid pregnancy. Historically, BBT measurements have offered retrospective data, helping confirm that ovulation has already happened and that the fertile window is closing or closed. But that may be changing thanks to Tempdrop’s machine learning algorithm (more on this below).
New study finds that Tempdrop confirms ovulation with comparable effectiveness to urine ovulation test kits
While only oral BBT thermometers have been clinically studied for effectiveness in measuring basal body temperature with the intention of avoiding pregnancy using the symptothermal method, many women have found it a hassle to remember to take their temperature at the same time every morning, before getting out of bed, drinking water, etc. Newcomers to the Femtech scene (like the Tempdrop armband, Oura ring, Ava bracelet, and other wearable thermometers) aim to match the effectiveness of oral thermometers while offering superior user-friendliness.
What distinguishes Tempdrop from other wearable thermometers
Tempdrop specifically measures underarm (aka armpit or axillary) temperatures because, per the study, “it measures the temperature of the skin above the axillary artery. This location is one of the places where skin temperature most closely resembles internal body temperature, as it is near a large blood vessel and if the measurement is taken for more than 12 min, it closely corresponds with the core body temperature.” (Anecdotally, when I worked in the hospital as an ICU nurse, we often checked axillary temperature on our patients who were unable to have their temperature taken orally. In fact, axillary temps were considered more reliable than oral readings.)
In the aforementioned 2025 Tempdrop study, 125 women, aged 18-45 and all living in the United States, tracked BBT overnight with the Tempdrop armband thermometer and also tested urinary luteinizing hormone (LH) and estrogen levels using the ClearBlue monitor. ClearBlue was the clinically validated control against which Tempdrop’s ability to identify ovulation was checked.
In the study, a sophisticated algorithm incorporating BBT readings was used to identify which cycle days were fertile vs non-fertile, as well as the day of ovulation, and they were confirmed by the ClearBlue results. Tempdrop performed well in terms of successfully identifying fertile days as well as non-fertile days, with a minimum of false positive days (days predicted to be fertile but were not) and false negative days (days predicted to be non-fertile but were fertile). In contrast, in a 2018 study the Ava bracelet wearable thermometer—which is worn on the wrist—was only able to retrospectively (after the fact) confirm ovulation rather than prospectively predict when ovulation would occur [3].
What’s next for integrating axillary temperature measurement into symptothermal method practice
Future research is needed to verify that Tempdrop’s algorithm can accurately anticipate fertile vs non-fertile days (based on previous cycle patterns plus machine learning) with comparable efficacy to ClearBlue and other urinary hormone tests. If this is confirmed, Tempdrop use could be formally integrated into symptothermal method protocols for pregnancy achievement or prevention.
Additionally, since the 2025 study was co-authored by Tempdrop founder Michael Vardi as well as the company’s Chief Technology Officer, further independent research by unrelated third parties is necessary.
What factors can skew BBT results?
It’s important to note that interrupted sleep, shift work (which throws off the body’s circadian rhythm), alcohol consumption, breastfeeding (since hormones can fluctuate often and in unpredictable ways during this time), and illness (particularly illnesses that cause fever) can all skew BBT results—even when taken orally.
Tempdrop claims that its product and algorithm specifically mitigates skewed results from sleep-related factors like sleep interruption, mouth breathing, restless sleep or sleeping at odd hours as for nightshift workers. (Of note: the 2018 study of the Ava bracelet measuring wrist temperature throughout the night found that its readings were not skewed by alcohol consumption and other non-sleep lifestyle factors. The Tempdrop website takes issue with the claim that skin temperature wearables, like the Ava bracelet, accurately reflect BBT, asserting that BBT must be measured closer to the body’s core.)
According to a December 25, 2025 blog post on the Tempdrop website:
“While you sleep [Tempdrop] collects thousands of data points, from the thermometer and an accelerometer that senses movement. When you sync to the Tempdrop app, a built-in algorithm filters out disturbances (like wake-ups, tossing, turning, and even nighttime [breast]feeds), zeroes in on your most restful moment, and delivers an accurate BBT reading.
That means even if you have irregular sleep, up with a baby, shift schedule, or simply restless nights, Tempdrop still gives you reliable BBT data for fertility awareness, cycle tracking, or trying to conceive.”
Can basal body temperature measurement help identify reproductive health issues?
Women will wonder, how might BBT data, as measured by Tempdrop or other wearable thermometers that sync with a user’s phone, help identify reproductive health issues? Are there patterns of temperature change with PCOS, endometriosis, early menopause, etc.?
No temp rise, no ovulation
Plain and simple, no observable temperature rise during a cycle is suggestive of no ovulation, meaning you’ve experienced an anovulatory cycle.
Particularly for women trying to conceive, this spells trouble, as there cannot be a baby without ovulation. The culprits behind anovulatory cycles range from hormonal imbalances (such as those that occur with PCOS), to stress, to hormonal contraception (remember, a bleeding episode while taking hormonal birth control is not a true period), to transitional seasons like onset of puberty or postpartum or perimenopause.
Low temperatures may signal a thyroid issue
Sometimes the basal body temperature baseline, or usual reading during the part of the cycle where temperature is expected to be low, is lower than normal. One potential cause is hypothyroidism. The Tempdrop website suggests that a pre-ovulation BBT consistently below 97.5 F is low, and therefore worth discussing with your doctor, who can screen for other symptoms.
Shorter luteal phase length may indicate a progesterone problem
Cycle trends as identified through the Tempdrop app may help women identify a short or shortening luteal phase (remember that the luteal phase is the second half, approximately, of the cycle, the time after ovulation and before menstruation). Estimates of how long a luteal phase should be vary, but generally 9 days or less is considered abnormal—with the exception of a return of fertility after childbirth, after which the luteal phase may be just a few days long but should lengthen with each consecutive cycle.
A short luteal phase may indicate low progesterone, which may occur downstream of some health issues and upstream of others, and is always worth exploring with a practitioner trained in restorative reproductive medicine.
Other potential health benefits of BBT tracking
In a video interview with Natural Womanhood Editor in Chief, Grace Emily Stark, Tempdrop founder Michael Vardi speculated about other potential health benefits of BBT tracking. Since the app measures sleep quality, Vardi suggested that a woman in her 40s might be clued in that she’s entering perimenopause by noticing that her cycle is beginning to shorten, and her sleep quality is beginning to decline.
Should FAM users just go straight to Mira or Inito?
Savvy Natural Womanhood readers may well wonder if, for the price of a wearable thermometer, it would be better to just purchase a Mira or Inito monitor. These quantitative machines provide actual numbers (not just a High or Low or Peak reading as with the ClearBlue monitor) for urinary hormone levels, which Tempdrop readings can only indirectly hint at.
But the specialized information that at-home lab testing provides is reflected in the price tag, ranging from $2-4 per stick for Mira users (depending on how many hormones are being measured), compared to the one-time cost of a wearable thermometer (and a nominal monthly fee for app users who choose the optional Tempdrop Premium experience). (For an in-depth discussion on who might benefit from the additional info provided by the Mira monitor, see Grace Emily Stark’s interview of Dr. Thomas Bouchard, MD.) And this ongoing cost is after the roughly $150 spent upfront for the monitor (less with Natural Womanhood’s affiliate code, AFNATURALWOMANHOOD).
The bottom line
The 2025 Tempdrop study indicates that oral thermometers may no longer be the only method for accurately measuring basal body temperature. Future research is needed to confirm the effectiveness of wearable thermometers (as part of the symptothermal method of family planning) for pregnancy achievement or avoidance. Perhaps most hopefully of all, the ease of use of wearables like Tempdrop may help increasingly larger numbers of women become more body literate and improve their reproductive health and overall wellness.