Longtime fans of the PBS period drama Downton Abbey assuredly remember the tragic death of young Lady Sybil from eclampsia after the delivery of her firstborn child in 1920. Prior to her delivery and death, Lady Sybil had exhibited signs of preeclampsia, which her family doctor had noted, but whose warnings unfortunately fell upon deaf ears. The memorable episode, poignantly acted by actress Jessica Findley Brown, left many viewers shaken, and was the source of much discussion in the media (and in at least one medical journal!) about the realities of obstetric care at the turn of the 20th century. Fortunately, research over the last 30 years has found that women, on the whole, are exhibiting fewer cases of mild preeclampsia than ever before. However, there have been dramatic increases in rates of severe preeclampsia, which can quickly progress to full-blown eclampsia–which, as the fictional Lady Sybil’s case demonstrated, can be a potentially fatal condition.
Recent research corroborates previous studies finding that women who conceive using a particular type of in vitro fertilization (IVF) known as frozen embryo transfer (FET) are at higher risk of developing a hypertensive (high blood pressure) disorder, like preeclampsia, during pregnancy [1]. While rising rates of obesity may be partly to blame for the increased risks of severe preeclampsia in the general population, the lack of a corpus luteum (an important by-product of the natural menstrual cycle) in women who utilize FET may make these women more susceptible to this potentially life-threatening complication.
IVF “Alphabet soup”
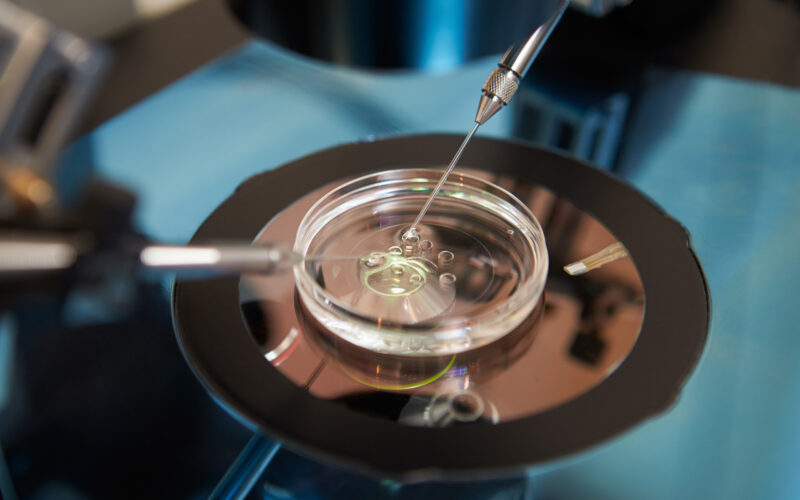
Women navigating the mainstream medical model of infertility treatment encounter a veritable alphabet soup as they consider their options for (hopeful) conception. Assisted reproductive technology (ART) is the umbrella term for “all fertility treatments in which the eggs or embryos are handled,” according to the CDC. In vitro fertilization (IVF) is a type of ART in which a sperm fertilizes an egg in a lab, outside either biological parent’s body. The egg could be a woman’s own egg or a donor egg*, and with her partner’s sperm or donor sperm*. IVF can also occur using “fresh” embryos, retrieved just a few days prior from the biological mother’s body, or using previously-frozen embryos (FET). IVF with FET typically occurs in one of two ways: either through a “modified natural” cycle or a “programmed cycle.”
*Note that preeclampsia risks are also heightened in IVF cycles that utilize donor sperm and donor eggs. For the fascinating role that semen may play in this phenomenon, check out this article from the NW archives.
Why might women choose to have frozen embryos implanted over fresh embryos?
In many countries, rates of IVF using previously cryopreserved embryos, known as frozen embryo transfer (FET), exceed rates of IVF using fresh embryo transfer. Women who undergo IVF with fresh embryo transfer are known to have increased risks of having low birth weight or small-for-gestational-age (SGA) babies [2]. Some women opt for IVF using FET, which isn’t associated with these risks, and which some doctors believe leads to a higher successful pregnancy rate. (In reality, googling “are fresh or frozen embryo transfers more successful?” shows what a mixed bag the opinions on the issue can be, with some claiming frozen embryos are less likely, more likely, or just as likely to lead to successful pregnancies as fresh embryos. Because of the wildly unregulated nature of IVF, good data on the outcomes of various procedures can be difficult to come by, and can vary widely from clinic to clinic.)
Additionally, it’s believed that freezing a woman’s embryos for later use can give her body a chance to rest (and to hopefully avoid developing the potentially deadly complication of ovarian hyperstimulation syndrome) after the physically and emotionally taxing process of getting her body to release multiple mature eggs at one time for harvest/egg retrieval (rather than one or two at a time as occurs with a natural conception).
Programmed vs. modified-natural vs. natural FET
As mentioned above, FET can happen within a natural cycle, or within cycles that are “programmed” or “modified natural.”
Natural cycle FET
FET with natural cycles means that the embryo transfer is timed after the woman naturally ovulates, which may be desirable in women who have normal hormone production and ovulation each month (who would theoretically be able to conceive naturally from a hormonal and/or ovulatory perspective, but perhaps have blocked Fallopian tubes). This route requires intensive monitoring, including frequent blood draws and multiple ultrasounds.
Modified-natural cycle FET
Modified-natural cycles are often proposed as an option for women who have some hormonal deficiencies and/or ovulatory dysfunction. Frequent blood draws and ultrasounds are utilized to track the woman’s cycle until the pre-ovulation luteinizing hormone (LH) surge is detected. Ovulation is then triggered with human chorionic gonadotropin (hCG) injections. After ovulation, thickening of the endometrial lining is achieved with progesterone injections, with the hope that it will ensure the successful implantation of the transferred embryo.
Here, it is important to note that in both natural cycles and modified-natural cycles, the woman’s body creates a corpus luteum.
Programmed cycle FET
Programmed FET cycles require the least monitoring and offer a “convenience factor” of being able to schedule an embryo transfer date. The woman’s underlying hormones (and cycle) are suppressed with medications. Estrogen is given to stop follicular maturation, so there is no ovulation. The endometrial lining is built up with progesterone to a certain point, and then the embryo is transferred.
Importantly, with programmed cycle FET, no corpus luteum is created.
Risks of Programmed FET
Many previous studies (9 of them are linked here!) have found that women with programmed cycle FET are at increased risk of developing hypertensive disorders (high blood pressure problems) during pregnancy, including potentially life-threatening preeclampsia. To put that into perspective, preeclampsia affects 3-6% of all pregnancies, according to a 2013 study [3].
A 2021 cohort study of 70,000 pregnancies from France’s national IVF registry found that increased risk of both preeclampsia and hypertension (high blood pressure) were significantly higher in women who underwent programmed FET vs. modified natural cycle FET or fresh embryo transfer. A press release from the June 2021 meeting of the European Society of Human Reproduction and Embryology, where the study was presented, read:
“Results showed a higher rate of pre-eclampsia with frozen embryos transferred in the artificial (i.e., prepared with hormone therapy) frozen cycle (5.3%) than in an ovulatory cycle (2.3%) or in fresh cycles (2.4%). The rates were found similarly distinct in pregnancy-induced hypertension (4.7% vs 3.4% vs 3.3%).”
What’s more, these results held even when researchers controlled for maternal characteristics like age, how many times the mom had been pregnant, smoking status, obesity, and history of diabetes, hypertension, endometriosis, polycystic ovarian syndrome, and/or premature ovarian failure.
According to the press release, study authors believe that “because results obtained in an [modified natural] ovulatory cycle appear not to affect the chance of pregnancy, preservation of the ovulatory cycle could be advocated as first-line preparation in frozen embryo transfers whenever the choice is possible.”
Why might IVF with programmed cycle FET increase a woman’s risk of developing preeclampsia and other hypertensive disorders of pregnancy?
Fascinating research from 2019 suggests that the absence of a corpus luteum could plausibly explain why women who undergo IVF with programmed FET are at higher risk of developing hypertensive disorders of pregnancy, particularly preeclampsia [4]. The study was conducted between 2011 and 2017 by researchers at the University of Florida and published in Hypertension. 683 women were studied in groups according to how many corpus luteums they developed: one group had no corpus luteum, another had one, and the third group had more than one (this is possible due to ovarian hyperstimulation during fresh embryo cycles).
According to the American Heart Association News:
“Researchers found that preeclampsia rates reached 12.8 percent in women receiving frozen embryos under a programmed cycle without a corpus luteum compared with 3.9 percent among women who had frozen embryo transfers under a modified natural cycle with a corpus luteum.”
What role might the corpus luteum play in preventing hypertensive disorders during pregnancy?
In programmed FET cycles, exogenous (from outside the body) estrogen and progesterone are administered, but not in a way that mimics the amounts released (and timing of release) from the corpus luteum after natural ovulation.
What else might be missing in a woman whose body doesn’t form a corpus luteum? As we previously noted, the corpus luteum is not only responsible for progesterone production. It also produces some estrogen as well as the hormones relaxin and inhibin. The University of Florida study researchers observed:
“Although estradiol and progesterone are replaced during a programmed FET or donor egg cycle in the first trimester, other vasoactive products of the [corpus luteum], which may be important for maternal cardiovascular adaptation to pregnancy, such as relaxin,13–16 are not administered. Deficient circulatory adaptations during early gestation have been linked to adverse pregnancy outcomes, including preeclampsia.12,17,18” [4].
Women who struggle to conceive have options other than IVF
Here, I’ve focused on specific risks associated with IVF with FET, especially the risks of serious complications like preeclampsia associated with programmed cycle FET, which are significantly higher than other forms of IVF. However, the unfortunate reality is that even with a “natural” or “modified natural” cycle, the IVF process is still not natural. It’s risky for moms and babies no matter whether fresh or frozen embryos are used (and we’ve covered some of those risks previously), and it is a costly, invasive procedure with no guarantee of success (although rates of success for younger women, in particular, have improved greatly in recent years).
Fortunately, restorative reproductive medicine (RRM) healthcare providers offer women hope for conceiving apart from risky assisted reproductive technologies like IVF and intrauterine insemination (IUI). While RRM is not a bulletproof “magic pill” cure-all for infertility, trained providers work with the woman’s body to optimize hormone levels and ovulation and address the underlying root causes, understanding that infertility is often “downstream” of a problem elsewhere in the body. Rather than “overriding the system,” RRM works in cooperation with the incredible natural design of the female body.
Therefore, the reality that the more “natural” the version of IVF, the less risky it may be for moms, makes good intuitive sense. It should also encourage women who are struggling with infertility and considering IVF that hope may instead lie best in seeking out a provider who can help them achieve their healthiest natural cycles possible.
References:
[1] Petersen, S.H., et al. (2022) Risk of Hypertensive Disorders in Pregnancy After Fresh and Frozen Embryo Transfer in Assisted Reproduction: A Population-Based Cohort Study With Within-Sibship Analysis. Hypertension. doi.org/10.1161/HYPERTENSIONAHA.122.19689. [2] Ibrahim Y, Haviland MJ, Hacker MR, Penzias AS, Thornton KL, Sakkas D. Elevated progesterone and its impact on birth weight after fresh embryo transfers. J Assist Reprod Genet. 2017 Jun;34(6):759-764. doi: 10.1007/s10815-017-0920-8. Epub 2017 Apr 17. PMID: 28417348; PMCID: PMC5445056. [3] Ananth C V, Keyes K M, Wapner R J. Pre-eclampsia rates in the United States, 1980-2010: age-period-cohort analysis BMJ 2013; 347 :f6564 doi:10.1136/bmj.f6564 [4] von Versen-Höynck F, Schaub AM, Chi YY, Chiu KH, Liu J, Lingis M, Stan Williams R, Rhoton-Vlasak A, Nichols WW, Fleischmann RR, Zhang W, Winn VD, Segal MS, Conrad KP, Baker VL. Increased Preeclampsia Risk and Reduced Aortic Compliance With In Vitro Fertilization Cycles in the Absence of a Corpus Luteum. Hypertension. 2019 Mar;73(3):640-649. doi: 10.1161/HYPERTENSIONAHA.118.12043. PMID: 30636552; PMCID: PMC6434532.Additional Reading:
IVF and Restorative Reproductive Medicine Stories: What they have in common, and how they differ
Study: Children born after common fertility treatment may have heightened cancer risk
The affordable, effective alternative to IVF that no one talks about
The dark side of the IVF industry, from a survivor
The hidden costs of IVF: heartbreak, health risks, and helplessness