I’m one of the lucky ones. I have never experienced a miscarriage. Both my children were carried to term with few complications and few of the usual pregnancy-related discomforts. No other mother I’ve met seems to have been so lucky.
According to the American Pregnancy Association, 10 to 25 percent of all clinically recognized pregnancies end in miscarriage. That means that if you and three friends each conceive, there’s a good chance that one of you will suffer such a loss. Most likely, you have a family member or a friend who has.
Women who experience this painful event are often told that “it just happens, but you can try again.” Unfortunately, many who have had one miscarriage go on to have several more, and fall into despair, feeling they will never bear a child.
But is the reason always unknown? It might be to the general public, but thankfully, miscarriage is not always such a complete mystery, and sometimes, it can be prevented. A growing number of physicians and Fertility Care practitioners are quietly working on interventions for miscarriage prevention related to a particular miscarriage cause—progesterone deficiency due to a luteal phase defect. Small but well-designed studies on women practicing fertility awareness have led some doctors to believe that a majority of miscarriages specifically due to luteal phase defects are preventable.
With fertility awareness, couples track what is happening with the woman’s cycle every day. The resulting chart provides a critical piece of information: the length of the woman’s pre-peak and post-peak phases. The pre-peak phase is the time between the first day of her period and the most fertile day of her cycle: the last day of what is called “peak type mucus” (the really fertile kind). After peak day the mucus consistency changes radically; this change is easily noticeable to women who have learned to chart. Then starts the post-peak phase, which lasts until the first day of the woman’s next period.
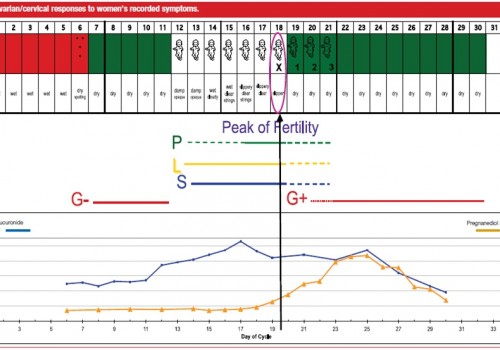
Over many years of observation, OB/GYNs and practitioners have noticed that women with shorter post-peak phases have a higher risk of miscarriage than their peers who have post-peak phases that consistently last from 9 to 13 days. Why is that?
For a pregnancy to be successful, the embryo must attach to the lining of the woman’s uterus and successfully implant there. During the post-peak phase, progesterone is the dominant hormone and plays a key role in thickening the uterine lining to prepare for implantation should conception occur. Progesterone helps the pregnancy survive and continue, especially early on, by decreasing the contractility (think: preventing contractions) of the uterine muscle and by altering immune function to fight off infectious threats. Women with short post-peak phases have low progesterone levels. The lack of progesterone at this particular time in the cycle can prevent successful implantation of the newly-conceived embryo. If the embryo does successfully implant, inadequate progesterone may lead to early pregnancy loss because immune system threats aren’t neutralized, and/or because the uterine muscle contracts and expels the embryo.

With fertility awareness, an effective miscarriage-reducing treatment can take place.
First, the problem can be identified: the short peak phase is noticed, then the progesterone levels can be tested during that phase and compared to normal levels. With this information, the medical provider can administer the strategic dose of progesterone. To be effective, the supplement must be taken after peak day, which is easy to identify when a woman charts.
Miscarriage may be preventable in the months following conception, if the mother has already been charting. She just needs to consult a fertility awareness practitioner who knows how to interpret indicators of progesterone levels. If it’s early enough in the pregnancy, the practitioner can start her on progesterone therapy immediately, based on her previous charting, and monitor her while she continues the therapy throughout the pregnancy. In some cases, this supportive therapy may allow for a healthy baby to be born.
Many of my friends say they owe their babies to fertility awareness and the diagnosis and treatment of a short post-peak phase. Progesterone is an incredible hormone! Besides helping the endometrial lining to support a pregnancy, it can also treat post-partum depression with similar rates of success.
Given that miscarriages are so common, especially in first pregnancies, I would strongly advise any couple who is planning to conceive to seek the help of a fertility care practitioner who is networked with an ob-gyn who knows how to administer progesterone therapy, should the need arise.
Learning to chart your biomarkers of fertility is surprisingly simple; I’m even teaching teens to do it. If such a simple habit can prevent a loss, why wouldn’t we want all women to have the opportunity to learn?
Something CAN be done to prevent some miscarriages. And the best part is, it’s nothing particularly invasive or difficult.
Please share this article with others. You never know who needs to read it.
Addendum: It’s important to note that cervical mucus is not the only biomarker of reproductive health that can predict risk of miscarriage. Basal body temperature can also be an indicator. There are several patterns of temperature shifts that are linked to progesterone deficiency. Reach out to a Fertility Awareness practitioner for more information.
This article was last updated March 30th, 2023 to clarify that miscarriages due to a specific cause, progesterone deficiency because of luteal phase defects, may be highly preventable with hormonal support. The specific ways that progesterone deficiency may contribute to early pregnancy loss were also clarified.








There are some serious errors in this post. Chemical pregnancies are not “pregnancies which occur while the woman is on birth control.” They’re pregnancies that miscarry before there is clinical evidence of pregnancy, i.e., seeing the fetus on ultrasound. So it is absolutely incorrect to say that using fertility awareness to avoid pregnancy would avoid all miscarriages of chemical pregnancies. That’s just a complete misunderstanding of what a chemical pregnancy is, demonstrating a poor grasp of basic information about miscarriages. Most such early losses are the result of genetic or chromosomal errors, factors over which a woman has no control. While hormonal issues such as insufficient progesterone or short luteal phases can be a cause, their role here is way overblown. FAM is great, but most miscarriages cannot be prevented in the way the author suggests. I imagine most women who have struggled to get pregnant or faced loss probably know this already. Still, it would be a shame for women suffering in this situation to feel that a miscarriage was their fault, based on this poorly researched post.
Tanka, thank you for reading this post and
holding us accountable for communicating accurate information. Please allow me to address the issues you raised about chemical pregnancies and the role of insufficient progesterone. First, chemical pregnancies – The American Preg Association states that “Chemical pregnancies may account for 50-75% of all miscarriages. This occurs when a pregnancy is lost shortly after implantation, resulting in bleeding that occurs around the time of her expected period. The woman may not realize that she conceived when she experiences a chemical pregnancy.” This was the definition I was working off of, which includes your understanding of the term in that yes, there is no evidence of the pregnancy by ultrasound, etc. It is a pregnancy that miscarried because it couldn’t implant or stay implanted, possibly due to outside agents that thin the lining of the uterus or try to prevent implantation all together. So, I think we’re both right. Likewise with
the role of hormonal imbalances like insufficient corpus luteum/progesterone. You are absolutely right that some inherent genetic factors may lead to miscarriage, absolutely – hormonal imbalances don’t account for everything. However, cervical mucus scoring as well as cycle length are lesser-known but equally valid evidence-based indicators of miscarriage risk, particularly repetitive miscarriages. This I learned directly from those who researched the natural method I teach. I would encourage you to visit http://www.naprotechnology.com/abortion.htm to find out more.