Welcome back for our second installment of “Reasons Women Need Periods,” a series dedicated to taking a deep dive into some of the reasons women actually need their cycles for optimal health. This week: Bone health and development.
When you think about cycling and menstruation, you don’t typically think about your bone health. But important research has emerged in the last few decades linking the natural cycle of women’s reproductive hormones to their bone health and development. That’s right, yet another thing your cycles are good for, is protecting your current and future bone health–which is especially important for women. Just another reason why, yes, you do “need” a period!
How bones work
We often think of our skeleton as a fixed structure, just there to hold our bodies upright. But the truth is that our bones are anything but static; they have a life cycle that involves building up, tearing down, and rebuilding tissue constantly. Kind of like construction at the LaGuardia airport.
Kimberly Reda-Wilson is a four-year apprentice in the program Bones For Life, which offers classes that “explore movement intelligence of bone strength and weight-bearing posture,” as a preventative measure against osteoporosis. Reda-Wilson explains, “Bones are living tissue. They have blood vessels and are made of living cells, which help them to grow and repair themselves. They are just as alive as your heart or brain or lungs.”
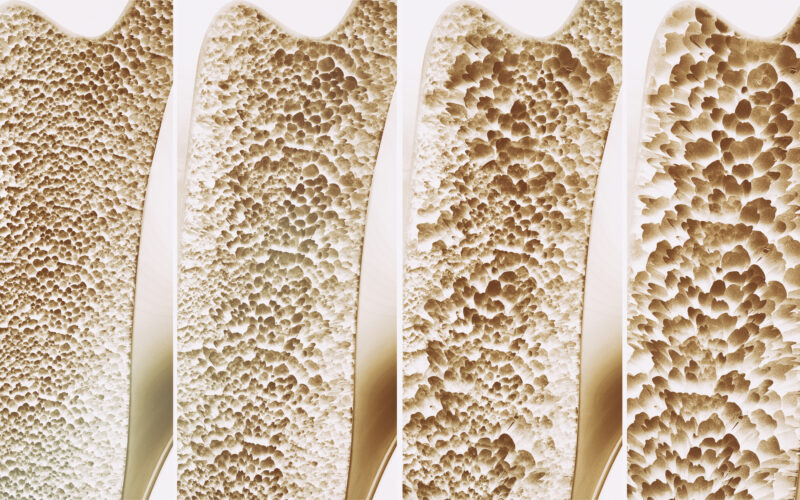
There are two main types of cells that comprise bone tissue: Bone forming cells and bone resorbing cells. The types of cells that form bone are called osteoblasts and osteocytes. The type of cells that resorb bone are called osteoclasts. Bone also contains nonmineral matrices of collagen and noncollagenous proteins called osteoids, as well as mineral salts. The higher your bone mineral content, the denser your bones are—which, as you might guess, is a good thing. The denser your bones, the less likely you are to experience fractures. Low bone density can lead to osteoporosis, a condition where bones become dangerously porous and fragile, increasing their risk of fracturing.
Hormones, cycles, and their roles in bone health & development
It is well established that estrogen plays a role in bone formation. The major physiological effects of estrogen are to inhibit bone resorption and to promote bone growth. For years, researchers have surmised that post-menopausal bone loss is attributed to the lack of estrogen that occurs after menopause. But estrogen isn’t the only thing post-menopausal women lack. After cycles cease, progesterone is low as well. Mounting research indicates that bones need progesterone just as much as estrogen.
In this 2010 research paper co-written by two of the leading researchers on reproductive hormones and bone health, Dr. Jerilynn Prior and Dr. Vanadin Seifert-Klauss, it was confirmed that “In vitro studies of human osteoblasts in culture, prospective studies in adolescent, premenopausal, perimenopausal, and post-menopausal women all indicate that progesterone—likely working through bone formation pathways—plays an active role in maintaining women’s bone and in osteoporosis prevention.”
Dr. Jerilynn Prior is the director of the Centre for Menstrual Cycle and Ovulation Research (CeMCOR) and her life’s work has been researching and educating about progesterone’s relationship to bone health.
“You need ovulation, as well as normal cycles, for healthy bones,” Dr. Prior told me in a virtual meeting. “Women spend the first 25 years of their lives building bone mass. If they are ovulating normally, they should be able to keep that bone mass throughout their reproductive life and beyond.”
That means post-menopausal bone health is decided by hormone processes that occurred decades earlier. “The story that everyone hears is that it’s estrogen deficiency that causes post-menopausal bone loss. But in reality, it’s the long time of pre-menopausal bone loss that’s silent if you’re not cycling regularly over the course of your reproductive years,” Dr. Prior explains.
In other words, if you’re not ovulating during your prime reproductive years, your bone density will be negatively impacted, and those effects will manifest in your post-menopausal years.
So, how can we support bone health for post-menopausal women? Dr. Prior says plainly, “You need to put bone mass in your bank in those [prior] critical years—and the only way to do that is by ovulating [regularly and functionally].”
Progesterone: the “heal and repair” hormone
Considering what we know about the effects of estrogen and progesterone in the body, Dr. Prior’s message makes intuitive sense.
We know that estrogen and progesterone have complementary effects on our reproductive and general health. Estrogen proliferates the endometrium and breast tissue, elevates blood sugar, dilates blood vessels, stimulates brain cells, and gives women a general boost of energy and feeling of well-being. Progesterone, estrogen’s alter ego, maintains endometrium tissue, relaxes blood vessels, normalizes blood sugar, maintains and heals brain cells, and promotes mood stabilization. We need both. Can you imagine being stimulated all of the time without the heal-and-repair mode?
So it should come as no surprise that the same is true of our bones. In this paper by Dr. Prior, she explains that, “when menstrual cycles are normal length and normally ovulatory, estrogen and progesterone are balanced and bone mineral density is stable. However, clinically normal cycles commonly have ovulatory disturbances (anovulation, short luteal phases) and low progesterone levels; these are more frequent in teen and perimenopausal women and increased by everyday stressors: energy insufficiency, emotional/social/economic threats and illness.”
Dr. Prior claims that the main contributor to ovulatory disturbances these days is … drum-roll … stress. “Women are expected to perform in the workplace the same as men. Yet, they’re also doing all the traditional things at home with little to no help. Women have an incredible burden today.” It’s true, women are under great demands emotionally, socially, culturally, financially, and physically in a fast-paced world. You could argue that women don’t get a “heal and repair” mode both hormonally and literally in their daily lives.
Synthetic hormones are not created equal
“Great,” you may be thinking. “I’m on hormonal contraception, and doesn’t that contain a form of progesterone? That should be good for my bones.” Unfortunately, you’d be wrong.
Hormonal contraception contains an artificial form of progesterone known as progestin. There are six different compounds of progestins used in hormonal contraception. But Dr. Prior warns that progestins do not have the same positive effect on our bone health (nor on our general health, either) as natural or bio-identical progesterone does. “Progestins do not have a class effect except for two things that are signified in their name,” Dr. Prior says. The first effect is “to preserve an existing pregnancy, and the other is to transform the proliferative effect of estrogen on the endometrium to a secretory one. Those are the only two things all progestins do.”
So, progestin in birth control may send a negative feedback signal to the part of the brain that wants to start a new cycle (the same thing that preserves an existing pregnancy), but it does not do anything to preserve your bones. In fact, it could actually be robbing them of a crucial opportunity to build bone mineral density.
Does hormonal contraception use negatively affect bone health?
Remember the ovulatory disturbances Dr. Prior talked about? As it happens, another huge correlation to ovulatory dysfunction is hormonal contraceptive use. One third of women who go on the Pill do so for solely gynecologic reasons, such as irregular or painful periods. These are usually glaring symptoms of an ovulatory dysfunction, which then goes untreated as a woman is prescribed birth control that masks the underlying dysfunction without actually doing anything to resolve it.
When I asked Dr. Prior if hormonal contraceptive use affects bone health, she gave a resounding “Yes!” After all, hormonal contraception creates an “ovulatory dysfunction” itself, in that it prevents pregnancy by preventing ovulation. Ovulation is the only thing that can produce progesterone, so if there is no ovulation, then—you guessed it—there is no progesterone. And we’ve already talked about how vital progesterone—the real stuff, not synthetic progestin—is for bone health and development!
It’s especially problematic for their future bone health when teenagers and young women start birth control. Since the teenage years are so critical for building bone, it is that much more important for adolescent girls to have normal menstrual maturation undisturbed by artificial hormones. “Birth control use in adolescent girls has been shown to be significantly negative for spinal bone gain,” says Dr. Prior. “That’s something everyone needs to know.” The detrimental effects of progestin on bone health for adolescent girls was confirmed in a 2001 study that focused on Depo-Provera use. The Depo shot, which comprises one high dose shot of medroxyprogesterone acetate (a progestin) every 3 months, also happens to be the highest progestin dose of all hormonal contraceptives. And, as shown by the study, it also happens to significantly decrease bone mineral density (BMD). This is just one more reason why women, and teenagers especially, need a (regular, post-ovulatory) period.
Cycles and stress-management: Keys to good bone health & preventing osteoporosis
So what does this mean for women hoping to maximize their bone health and maybe even evade osteoporosis?
Dr. Prior makes the point that perimenopause and menopause—and the bone density loss they come with—are very normal parts of life. If a woman has had the opportunity to cycle normally through puberty and onward, she should be well-equipped to withstand the natural loss of bone density that occurs in those years. And Dr. Prior makes it clear that while estrogen is important, progesterone deserves its 15 minutes of fame, too. “Although the dominant osteoporosis paradigm for women is, and should remain, centered on estrogen, progesterone is emerging as an important partner hormone that collaborates with estrogen,” she says.
Kimberly Reda-Wilson’s work with Bones for Life focuses on women in the post-menopausal years, and the things women can do to combat osteoporosis as they age. “While there are common denominators (diet, exercise, and stress management) among bone loss prevention programs, each one seems to emphasize a different component,” Reda-Wilson explains. “Originally the Women to Women’s program (now Women’s Health Network) emphasized an alkaline-based diet, exercise, supplements, and stress management. The Save Our Bones program also emphasizes an alkaline-based diet, exercise, supplements and stress management,” she says.
There it is again . . . the word stress! Both Reda-Wilson and Dr. Prior agree that stress management is a huge component in osteoporosis prevention. Of course, not all stressors are within each individual woman’s control—in fact, many stressors could be systemic, cultural, and political. But healthy stress management is certainly something healthcare providers should prioritize discussing with their patients. If women can bring down the stressors in their life, cycle naturally, and minimize ovulatory dysfunctions, it is quite reasonable to expect their bone health to benefit.
So there you have it. Having a period improves your immune system (as we discussed last week, here), and it also improves your bone health. These are two pretty darn good reasons women need their cycles–that is, they need to ovulate and have periods–for optimal health, and why Fertility Awareness-Based Methods (FABM), which allow women to cycle naturally while planning their families with high effectiveness rates, are far superior to contraception when it comes to safeguarding women’s health while preventing pregnancy.
Stay tuned for more in our “Reasons Women Need Periods” series in the coming weeks.
Did you learn something from this article? We hope so! Help us educate more women about their cycles and fertility by donating to our cause today. And check out the following resources for more information on the benefits of Fertility Awareness Based Methods:
Reasons Women Need Periods: The Role of the Menstrual Cycle in the Immune System
The Powerful Link Between Fertility Awareness and Mental Health