Menopause is not typically a word women like to hear. Whether it’s pre, peri, or simply just menopause.
Regardless of when the ovary releases the final egg, cycles make a major shift around the mid-thirties, leading to a large drop in fertility after age 35 (generally speaking, as every woman is different). De-regulation of cycles—and the ultimate cessation of them (menopause)—can be a decade-long process. The following are a few key points women in their late thirties and forties can keep in mind to protect their future health, and make for a smoother transition into menopause.
What changes for women’s cycles and fertility after 35?
Think of your ovary as a bag of popcorn. When you first put it in the microwave, there is nothing. Think of that as the time before puberty. Then the popcorn starts to pop – hormones wake up, but not necessarily at a regular rate. Then in your twenties the popcorn is at peak height of regularity and is generally copious. Pops everywhere. But as time goes on, the popcorn pops space out a little more and become less regular. This is called premenopause, which can take up to 10 years! The final, feeble pops are perimenopause, which is usually the final year or two before menopause, when eventually, no more pieces of popcorn remain to pop.
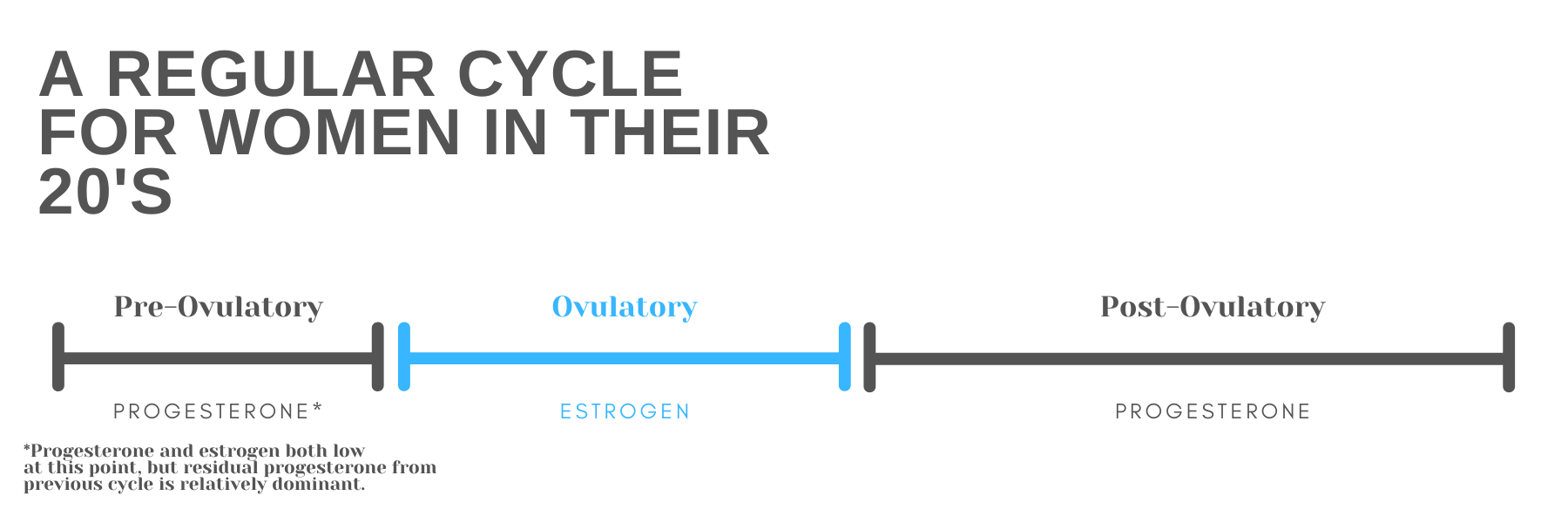
During pre and peri menopause, there tends to be a little more space between the “pops” (eggs being released) and some months there simply isn’t a pop (called an anovulatory cycle). Because of this, estrogen tends to take a more dominant seat. Estrogen is a necessary hormone that follicles pump out as they grow in the ovary during the ovulatory, or fertile, time. The longer it takes to ovulate, the longer the exposure to estrogen. And the only thing that can counter balance estrogen is progesterone, the post ovulatory hormone. Unfortunately, shortened post ovulatory phases are often the first part of cycle de-regulation. Therefore there simply isn’t enough progesterone to counter the higher levels of estrogen. To balance out a cycle, typically there should be a 1:3 ratio of estrogen to progesterone.

Still with me?
With this estrogen dominance, symptoms like weight gain, fibrocystic breasts, constant and difficult-to-read cervical mucus, irregular bleeding, insomnia, lower libido, and thyroid dysfunction are commonly reported. So what’s a woman to do? Here are the 3 most important things you can do today to make your transition through pre, peri, and menopause a little smoother, and successfully navigate your fertility after 35.
Put your best foot forward when it comes to your health
Women over 35 navigating their cycles can benefit from considering the following changes: lifestyle and nutrition changes, fertility support (for those who need it), and medical support. Mid-thirties cycle changes are more or less a given, but the disruptions they can cause in your well-being don’t have to be.
Lifestyle and nutrition changes
Veggies have always been important, but at this stage, they are even more important. There are major estrogen receptors in the GI tract, so if your diet doesn’t contain enough fiber to break down and move stools, there will be excess estrogen sitting around in your bowels.
Cardio and Strength training even just 3 hours a week can decrease estrogen levels. Research shows that exercise can increase levels of a protein called sex hormone-binding globulin that binds up free-estrogen in the serum. You don’t need a gym membership if that feels overwhelming to you. You can buy some dumbbells or stretch bands and find some great YouTube workout videos from the comfort of your own home.
Decrease stress levels (aka decrease cortisol, which competes with progesterone—which is the only hormone that can “balance” estrogen). If you haven’t already, try taking up some form of meditation/prayer/mindfulness which can be a powerful piece of lowering stress. You can join a local group or try it at home on your own.
Consider your Family-Planning Wishes
Average U.S. maternal ages have been rising since the 1980s. Many women in their late thirties are just starting to try to conceive at this point. Menopause is just about the last thing a woman wants to hear about when she’s anxious to start a chapter of motherhood.
If achieving pregnancy is proving to be difficult, try working with a handful of practitioners who are experienced in the pre-menopause years. (Can we please get a better name for this season?) This can include acupuncturists, fertility awareness instructors, and medical management physicians who are fluent in fertility charting and its implications. IVF, which is the common solution in this situation, can exacerbate premenopause symptoms and even lead to problems with post-menopausal health. (1)
Make peace with the changes that will likely arise in your fertility after 35. If you always thought you wanted “one more kid,” this is the time to think critically about those expectations and make peace with your reality. It’s a lot easier to make decisions now; after cycles cease it will be too late.
Get Medical Advice and Support
Many practitioners tout the use of bio-identical progesterone creams. I can only recommend this under the supervision of medical care, but it’s worth asking your doctor about it.
Find your “premenopausal team” (okay, maybe we can call it the wise woman team?). Utilize herbalists, counselors, and other practitioners who make you feel comfortable and cared for. If anyone tells you, “This is just how it is,” and you aren’t satisfied, now is the time to say, “I’m moving on.” You decide your care!
While you may feel overwhelmed by all this “menopause business” there is no better time than the present to take charge of your health and wellness.
¹Perimenopausal changes are similar to changes caused by some infertility treatments. In vitro fertilization (IVF) requires laparoscopic surgery (through a small tube in the abdomen) to suck up ovarian egg cells that are nearly ready to ovulate so they can be grown and fertilized in a laboratory and then injected into the woman’s uterus. In order to collect the maximum number of eggs, gynecologists override inhibin using a technique called “ovarian hyper-stimulation.” The woman is given daily injections of FSH until many follicles have been stimulated and estrogen levels are very high. She is then injected with another hormone (much like luteinizing hormone [LH], another pituitary hormone that stimulates the ovary) to mimic the normal mid-cycle LH surge and this triggers ovulation.
For additional reading:
“Before the Change: Taking Charge of your Perimenopause” by Ann Louise Gittleman PHD CNS
“Life Phases: Premenopause” by the Centre for Menstrual Cycle and Ovulation Research






