Intrauterine devices (IUDs) are promised to women as a “set-it-and-forget-it” form of birth control. No daily pill to take, no maintenance…there’s even the promise of light and easy periods or periods that disappear altogether. According to the advertising, a woman with an IUD shouldn’t have to think about the device at all for 5-10 years or until she’s looking to get pregnant. However, one common side effect of IUDs can make it rather hard to forget: continuous bleeding.
There are four brands of hormonal IUDs available in the U.S., Mirena, Skyla, Liletta, and Kyleena. Each works as contraception by thickening cervical mucus (to prevent sperm from swimming to the egg) and thinning the uterine lining (to make it difficult for a newly conceived human to implant). It’s this second mechanism that’s related to symptoms like the breakthrough bleeding that many women experience with the IUD.
How common is continuous bleeding with a hormonal IUD?
IUD brand Mirena lists changes in bleeding as one of their common side effects. They state “you may have bleeding and spotting between menstrual periods, especially during the first 3 to 6 months. Sometimes the bleeding is heavier than usual at first.”
According to ACOG, breakthrough bleeding (bleeding that’s not part of your period) can happen with any type of birth control but is more common with certain types. The “certain types” are low-dose birth control pills, the implant, and hormonal IUDs like Mirena. With IUDs, it may take 2 to 6 months for irregular bleeding to subside.
A Reddit thread on “Mirena IUD: never ending period…” has firsthand accounts of women who’ve experienced frequent or continuous bleeding after IUD insertion. For some women, this side effect lasted several weeks, while other women reported frequent bleeding for an entire year before deciding to make a new birth control plan with their OB/GYN.
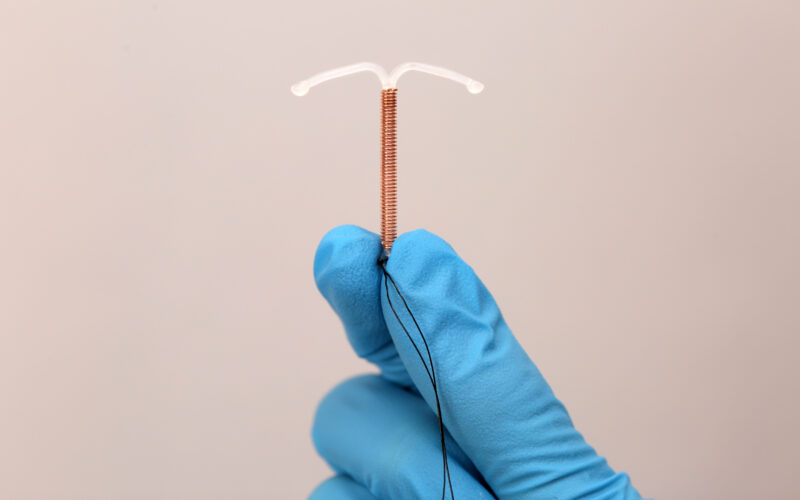
What about copper IUDs?
Although copper IUDs do not use synthetic hormones, the effect they produce is similar to hormonal IUDs. Copper is a naturally cytotoxic metal (meaning toxic to cells) and damages sperm [1]. Like the hormonal IUD, the copper IUD also creates an inflammatory response within the uterus. Heavier, longer periods are common side effects of copper IUDs, and the Paragard website also lists spotting between periods as a common side effect. A Healthline article warns that Paragard may be particularly inappropriate for some women with uterine fibroids because it can make their bleeding heavier and more painful.
The mechanism for why IUDs cause bleeding is difficult to determine, especially since recent research into the negative effects of IUDs is rather sparse. This report from 1980 provides a clue, however [2]. It states that IUDs increase local fibrinolytic (meaning blood-thinning) activity that makes it difficult for bleeding to stop. There’s also the physical reality that there is a foreign body in the uterus that can cause pressure or irritation to the uterine walls and cause bleeding.
Is continuous bleeding a serious problem?
On its own, continuous bleeding may not be serious. Many women see an improvement in symptoms after 2 to 6 months without further complications. If bleeding is frequent or heavy enough, women may need to take an iron supplement to treat IUD-caused anemia.
According to Drug Dangers, the FDA has received over 45,000 reports of IUD-related bleeding complications. They also note that a concern with continuous bleeding is that it may mask the early warning signs of other serious complications such as an ectopic pregnancy, displaced IUD, or infection or even uterine cancer. Without early detection, these complications could become life-threatening.
Reality vs. what IUD companies promise
Pharmaceutical companies advertise a low-dose hormone (Mirena) or hormone-free (Paragard) option for pregnancy prevention. According to Mayo Clinic, Mirena is also considered a good treatment option for women with heavy or painful periods, endometriosis, anemia, and fibroids.
In reality, an IUD may actually complicate periods by increasing bleeding and introducing breakthrough bleeding. In addition, the risk of unexpected pregnancy may be higher than originally thought. Rather than being worry-free, IUDs may come with additional difficulties such as anxiety, depression, or severe reactions.
One of the most difficult parts of an IUD experience gone wrong is that a decision that promised to give a woman more control over her body leads to her feeling less in control than ever before. Luckily, women don’t need to “control” their bodies to treat reproductive symptoms or prevent pregnancies. Learning a fertility awareness method can provide the knowledge and empowerment to understand your body and learn the root cause of reproductive or hormonal problems, without any side effects.
This article was updated on January 27, 2025, to note that copper IUDs may be inappropriate for women who experience pain and/or bleeding due to uterine fibroids. The copper IUD’s effects can worsen the pain and increase the bleeding.
Additional Reading:
IUDs: Of (insertion) pain and (uterine) perforation
Heavy bleeding, anxiety, and other signs your IUD is not good for you
References:
[1] Makler A, Zinder O. The effect of copper on spermatozoal motility and viability evaluated objectively with the aid of the multiple-exposure photography method. Am J Obstet Gynecol. 1980 Sep 15;138(2):156-64. doi: 10.1016/0002-9378(80)90027-7. PMID: 7191636. [2] Lu Q. [Fibrinolytic activity in endometrium and uterine fluid of women using intrauterine contraceptive devices]. Shengzhi Yu Biyun. 1983 Aug;3(3):6-8. Chinese. PMID: 12267402.