When it comes to periods, misinformation abounds. Periods and period research have long been stigmatized, so it’s no surprise that so little is known about periods, or why women have them. Purveyors of hormonal contraception like to tell women that there’s no need for them to have a period, but more and more, researchers are discovering that is simply not true. Although science has only begun to scratch the surface of this important topic, there are myriad reasons why cycling naturally—that is, having a menstrual cycle free from the influence of artificial hormones—is important for the health and development of women. This is the first post in our series, “Reasons Women Need Periods,” where we delve into some of the reasons women actually need their cycles for optimal health. First up: The immune system.
You could say that the immune system is having a moment right now. Perhaps even more than 15 minutes of fame.
Now there’s a lot we don’t know about microbes, gut flora, and the immune system. In many ways, it is comparable to what we know about outer space. We have a vantage point and some thoughts and theories, but the study of immune-system functions and dysfunctions is a vast and almost immeasurable expanse.
Female reproductive hormones and their role in immunity
One of the great mysteries for immunologists is the different immune responses in men and women. Women are known to respond to infection, vaccination, and trauma with increased antibody production and a more T helper (Th)2-predominant immune response, whereas a Th1 response and inflammation are usually more common in men. Th1 and Th2 are subsets of T helper cells, which are responsible for responding to potential threats to the immune system. Th1-type cytokines tend to produce pro-inflammatory responses and Th2-type cytokines have more of an anti-inflammatory response.
The only conclusion to draw here is that sex hormones somehow play a role in the immune system.
In a normal fertility cycle, estrogen and progesterone act in a cyclical manner. Immunity seems to follow suit. In the follicular phase (the first half of the cycle) estrogen is dominant. Since estrogenic cervical fluid “opens up” the reproductive tract to sperm (and therefore other foreign microbes) during this phase, the immune system needs to be on high alert to filter out potential invaders.
In the luteal phase (the post-ovulatory phase of the cycle), progesterone is dominant. During this phase, gestagenic cervical fluid seals the cervix up (as well as the rest of the reproductive tract) and immunity is temporarily suppressed; this allows the body to accommodate a potential pregnancy. Pregnancy, after all, is an immunity conundrum; in any other scenario, the body would attack the arrival of a separate entity. Thanks to progesterone, the body has a workaround so that the immune system gives the baby a hall pass to stick around inside mom’s body for a bit. Otherwise, in a healthy, functioning immune system, pretty much everything is geared toward defending the body against anything that isn’t, well, her body.
Cycle phase impacts immune cell signaling
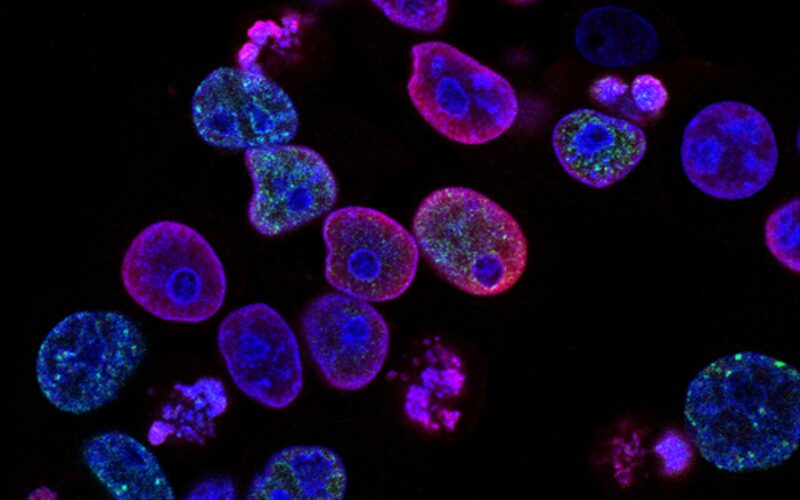
While research studies often require that female participants be on some form of contraception (which makes some logical sense in the case of, say, testing a medicine that may or may not harm a preborn baby), a 2022 systematic review and meta-analysis conducted by the University of Washington School of Medicine showed why studying naturally cycling women is key. Researchers found that concentrations of 53 different kinds of immune-signaling molecules called cytokines fluctuated depending on the woman’s menstrual cycle phase.
According to the study, “Many immune mediators were lower in the luteal phase, including chemokines, antibodies, matrix metalloproteinases, and several interleukins,” which is consistent with a lowered immune system during the luteal phase to prep for a potential baby.
Importantly for future research in all areas of women’s health, senior study author Dr. Florian Hadlik commented, “Scientists need to design their studies to make sure that all participants get measured at the same stage of the cycle.”
Cycle phase and autoimmune diseases
In autoimmune diseases, the immune system turns from attacking outside sources and turns toward attacking the body itself. Examples of autoimmune diseases are Crohn’s disease, Rheumatoid Arthritis, Lupus, Psoriasis, and Hashimotos. Eighty percent of people affected by autoimmune disease are female. That’s not a coincidence, and it’s certainly worthy of more scrutiny.
Just as the immune system operates cyclically in healthy women, many women with autoimmune diseases also notice a cyclical pattern of symptoms that coincides with their fertility cycle. For example, some notice a relief in symptoms post-ovulation as progesterone dominates the cycle, and an increase in symptoms right before menstruation as progesterone rapidly declines. Likewise, an increase in autoimmune symptoms may also occur during the follicular phase (ovulatory phase), when estrogen dominates the cycle.
The role of cervical fluid in immunity
Cervical fluid, that stuff on your underpants that is responsible for every human on the planet, is not just a sign of fertility—it is also another vital part of our immune system and is rich in immunoregulatory proteins. When a woman is in the infertile phase of her cycle, gestagenic cervical mucus seals up the cervix, keeps out all pathogens (including even semen), and fights off infection. When a woman is fertile and nearing ovulation, cervical mucus feeds and nourishes sperm and filters out the slow and malformed sperm.
The cervix—which is of course responsible for the production of cervical mucus—doesn’t fully mature until a woman is in her mid-twenties. That’s because the female fertility cycle (which doesn’t begin until puberty) plays a major role in cervical maturation. The exposure to cyclical immunity and hormonal fluctuations from the fertility cycle allows the cervix to undergo proper epithelial development, and develop a natural resistance to infection. Therefore, a cervix that has matured under these natural hormonal processes is pretty good at fighting off infections like human papillomavirus, also known as HPV.
How does hormonal contraception affect immunity?
Now that we’ve established how important the fertility cycle is for proper immune system development and functioning, it should be obvious that anything that disrupts fertility probably has an effect on our immune systems, too. Hormonal contraception works to override cycles with synthetic hormones, so it makes sense that hormonal contraception has an effect on the immune system and gut microbiota. Therefore, birth control may also have an effect on our chances of contracting both bacterial and viral disease.
When a woman is taking hormonal contraceptives, the cyclical effects of immunity cannot occur, because of the “leveling out” effect of the continuous dose of synthetic hormones. A woman on hormonal contraceptives receives a daily, small spike of artificial progesterone (called progestin), as well as estradiol if on the combination pill, which sends a negative feedback signal to the pituitary gland.
People often promote the adage that hormonal contraception tricks the body into thinking it is pregnant—but that’s not quite right. Instead, it is more accurate to say that hormonal contraception tricks the body into thinking ovulation already happened. But progestin, the artificial form of progesterone, doesn’t have the same beneficial effects on the body as progesterone—including temporary immune suppression.
Further, the use of hormonal contraceptives has been linked to changes in the functional capacity of immune cells in genital mucosae and altered levels of cytokines, chemokines, and antiviral factors in cervical fluid.
One of the ways hormonal contraception prevents pregnancy is by changing the structure and form of cervical fluid. It makes cervical fluid indefinitely inhospitable to sperm (rather than cyclically) but also alters the chemical level, cytokines, and immunological properties of the cervical fluid as well. If a woman takes hormonal contraception for an extended amount of time, the cervical crypts that produce cervical fluid alter and ultimately shrink (the clitoris shrinks too!) since they are no longer producing estrogenic cervical fluid in response to ovarian hormones.
Because cervical mucus is not just a sign of fertility, but also a vital part of our immune system, changes to cervical fluid caused by hormonal contraception may compromise one’s immunity to both reproductive infection and systemic infection.
Finally, remember how the exposure to cyclical immunity and hormonal fluctuations from the fertility cycle allows the cervix to develop a natural resistance to infection? Well, a little known effect of hormonal contraception is that it artificially accelerates the maturation process of epithelial tissues, exposing young women to increased susceptibility to infection.
The benefits of fertility awareness for building immunity: How cycling naturally could even be protective against severe COVID-19 outcomes
It’s clear that hormonal contraception affects much more than our ability to get pregnant. The impact of hormonal contraception on women’s immune systems is just another reason why promoting regular, healthy, and balanced hormones should be the gold standard of care for women. Menstrual cycles are so much more than just about reproduction, which is why using fertility awareness methods (FAM) or natural family planning (NFP)—which allow women to cycle naturally—has benefits beyond family planning.
Recent research has even discovered that a woman’s cycle could be protective against succumbing to COVID-19. It is well known that younger women tend to fare better with COVID-19 than do younger men, with women as a whole having comparatively lower mortality and lower morbidity from the disease. But because post-menopausal women (that is, women who no longer ovulate) with COVID-19 do not fare much better than men of the same age with the disease, preliminary research suggests that the high levels of a certain form of a naturally occurring estrogen (estradiol) found in women who still ovulate might offer younger women protection against severe COVID-19 outcomes.
Researchers think estradiol may be protective against severe COVID-19 outcomes because estradiol is known to regulate cytokines, proteins that play an important role in immune functioning. Severe cases of COVID-19 can incite what is known as a cytokine storm, an overreactive immune response that can be deadly. As a FEMM article detailing the estradiol/COVID-19 research put it, “this study is a reminder that women’s reproductive health can never be separated from overall health and wellbeing.”
Natural cycle maturation, free from the influence of synthetic hormones, allows reproductive tract tissues to develop and cervical mucus to produce, all of which make women’s bodies better suited to fight infection and inflammation. As a result, a woman’s health is best served when her body is allowed to ovulate and menstruate naturally, and when any hormonal disorders have been addressed with restorative reproductive medicine.
In the face of the COVID-19 pandemic, countless women and couples are facing changing needs for family planning and reproductive help. Click here to find Telehealth options for fertility-awareness-knowledgable doctors and medical professionals who can help you during this time.
Want to learn more about the impact of birth control on our bodies, and the benefits of cycling naturally? Check out these articles:
A Case for Organic Birth Control
FDA Citizen’s Petition on Birth Control: Shocking Stories of How Women Are Getting Hurt
What’s the good news about cervical health?
Getting to Know Synthetic Estrogens and Progestins: What Do They Do to Our Bodies?
The Surprising States of the Uterus Explained
Women can’t turn to fertility awareness, both as a diagnostic tool and an alternative to hormonal methods of family planning, if they don’t know about it. It is our goal at Natural Womanhood to give proper education to all women (and men!) to allow them to make informed choices about their reproductive and general health. Please consider donating to support our work so we can provide fertility awareness education to those seeking it, and contact us if you are in need of access to affordable fertility awareness education or a FABM-trained doctor.
When this article refers to fertility awareness methods (FAM), or natural family planning (NFP), we are referring to Fertility Awareness-Based Methods, evidence-based methods of cycle charting which can be used as effective forms of natural birth control when learned by a certified instructor.
This article was originally published on April 30, 2020. It has been updated to offer more resources and recent research.