When it comes to women’s reproductive health, much of the conversation revolves around the ovaries and uterus—but what about the tiny, powerful tubes connecting them? The fallopian tubes may not get much attention, but they play a critical role in fertility, conception, and overall reproductive well-being.
Whether you’re trying to get pregnant, trying pas to get pregnant, or simply want to better understand your body, knowing how your fallopian tubes function is key.
What are the fallopian tubes, and what are they for?
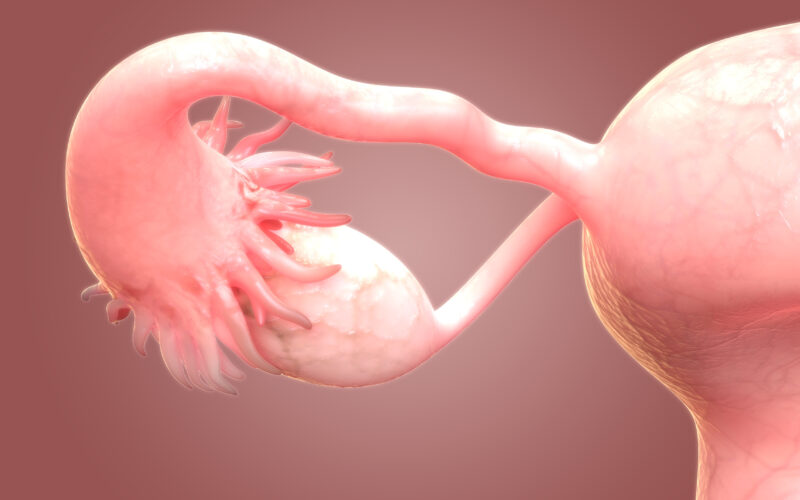
The female body’s two fallopian tubes (sometimes called uterine tubes or oviducts) are small ducts, or corridors, that connect each of the two ovaries to the uterus [1]. They don’t directly attach to the ovaries, but have finger-like ends that rest on or near the ovary. When your body gets ready to ovulate, an egg is released from one of the ovaries and uses the adjacent fallopian tube as a passageway to the uterus.
Once released, the female egg only survives for about 12-24 hours in the fallopian tube before beginning to disintegrate (if it’s not fertilized). If the egg is fertilized by sperm in the fallopian tube, conception results. That’s right, conception doesn’t happen in the uterus. It happens in one or the other fallopian tube [2]! The newly-conceived life (now called a zygote) then makes its way through the tube into the uterus, where implantation can occur, and a pregnancy begins.
If the egg is fertilized by sperm in the fallopian tube, conception results. That’s right, conception doesn’t happen in the uterus. It happens in one or the other fallopian tube!
Fallopian tube anatomy
Proper anatomy and functioning of the fallopian tubes is therefore crucial to female fertility.
Despite being a mere 10-12 centimeters (about 4-5 inches) in length and 1-4 millimeters (about 1/10th of an inch!) in diameter, each fallopian tube has four distinct parts, or regions. The infundibulum is the trumpet-shaped part closest to the ovary, and includes the finger-like projections called fimbriae that reach out to the ovary. These fimbriae catch the egg once it’s released. The ampulla is a large channel partway down the fallopian tube where fertilization happens. The isthmus is a tiny channel that connects the ampulla to the intramural portion, which is the last part of the tube; the one closest to the uterus.
Movement and nutrition: the fallopian tubes’ main gigs
The fallopian tubes are responsible for providing a physical meeting space for fertilization to occur et creating an optimal environment for fertilization–albeit for a very short window of time. Two specialized kinds of cells (ciliated and secretory cells, respectively) in the inner lining of the fallopian tubes make these functions possible [3].
The secretory cells produce fluids that nourish both the egg and sperm cells. The coordinated movement of the cilia (fine hairlike structures coming off ciliated cells), along with smooth muscle contractions in the tube, aid in moving the egg (or the zygote, if conception has occurred) from the ovary toward the uterus. Without the coordinated movement of the tube’s cilia and smooth muscle contractions (i.e., proper tubal motility), the zygote wouldn’t make it to the uterus for implantation, which would lead to a tubal grossesse extra-utérine (i.e., implantation within the tube itself) or the very early death of the new life before implantation can occur.
Without the coordinated movement of the tube’s cilia and smooth muscle contractions (i.e., proper tubal motility), the zygote wouldn’t make it to the uterus for implantation, which would lead to a tubal grossesse extra-utérine (i.e., implantation within the tube itself) or the very early death of the new life before implantation can occur.
If conception occurs, the zygote’s journey through the tube down to the uterus for implantation takes about a week. During this short time, the newly-conceived life undergoes rapid fire transitions through multiple developmental stages, from zygote to blastomere to morula to blastocyst [2].
Common issues impacting fallopian tubes
Various health conditions can involve or negatively impact the fallopian tubes, either by causing blockages within the tubes or impairing tubal motility (or doing both). Treatment options for each will be covered in detail in a forthcoming article on tubal factor infertility.
Blocked and immobile tubes
Perhaps the most common concern with fallopian tubes is for blockages (also known as occlusions). About 1 in 4 women with infertility have some form of tubal blockage, and there can be several underlying causes (many of which can also impair tubal motility). Blocked tubes are also a major contributor to subfertility, or difficulty getting pregnant. Blocked or immobile tubes can prevent sperm from reaching, and fertilizing, an egg. Or, if fertilization has occurred, a blocked or immobile tube could prevent the zygote from reaching the uterus. This is also one possible cause of a tubal ectopic pregnancy.
The conventional treatment option offered for tubal blockages is surgery to remove the blockage (or perhaps even the entire tube), sometimes followed by in vitro fertilization (IVF) if pregnancy is desired. In contrast, the restorative reproductive medicine approach focuses on opening the tube (i.e., removing the blockage) and/or restoring tubal mobility while keeping the tube intact. This approach preserves a woman’s fertility and restores her ability to conceive naturally. The specific treatment in each case depends on the cause and location of the blockage.
Fluid buildup
The fallopian tubes could also become blocked by fluid buildup anywhere along the length of the tube. If it’s closest to the uterus (the intramural portion mentioned above), it could be due to debris, tubal polyps, tubal muscle spasm, or scar tissue. A blockage in the middle region of the tube could be the result of a prior tubal ectopic pregnancy, tubal ligation, or endometriosis (more on these below). A blockage in the end of the fallopian tube farthest from the uterus (the infundibulum) may also cause a fluid buildup in the second portion, or ampulla, and this is called hydrosalpinx. Hydrosalpinx may result from severe endometriosis or pelvic inflammatory disease (PID).
Endométriose
Endométriose refers to endometrial-like tissue (that is, tissue similar to the endomètre, the lining of the uterus) that grows à l'extérieur the uterus. Like endometrial tissue, which is shed during your period each cycle, endometriosis lesions also bleed during “that time of the month.” But because it n'est pas located in the uterus, endometriosis tissue is not shed, causing pain and potentially scarring and adhesions (abnormal fusion of tissues to each other or other nearby organs). One place endometriosis tissue can grow is within or upon the fallopian tubes, often causing a blockage. Endometriosis affects up to 10% of women of reproductive age and is a major cause of infertility.
While hormonal contraception is often prescribed for symptom relief, it can’t cure endo. The gold standard treatment for endometriosis is excision (not ablation) surgery, performed by a surgeon who is an expert in endometriosis. When a surgeon trained in near-contact and other surgical techniques practiced in NaProTECHNOLOGY operates on a woman with endometriosis, lesion recurrence (grow back) rates may potentially be far lower than if a woman seeks care from a conventionally trained reproductive surgeon [4].
Inflammation
Inflammation of the fallopian tubes is called salpingitis. Salpingitis is visible inflammation of the fallopian tubes and is a component of pelvic inflammatory disease (PID) [5]. Often, inflammation results from a sexually transmitted infection like chlamydia or gonorrhea that has traveled upward through the reproductive tract. Left untreated, inflammation in the fallopian tubes can increase the risk of ectopic pregnancy and infertility.
Salpingectomy: surgical removal of the tubes
While the fallopian tubes are crucial for female fertility, there are some cases when surgical removal of the tubes may be recommended. Sometimes, conditions can be treated by a salpingostomy, or a small incision into the fallopian tubes. Other times, complete surgical removal of the fallopian tube—or salpingectomy—is needed.
Salpingectomy to reduce ovarian cancer risk
Women who have a BRCA1 or BRCA2 mutation may consider getting their fallopian tubes and ovaries removed. These are genetic mutations that are known to increase your risk of breast, ovarian, and fallopian tube cancers. But how would you know if you have one or both of these mutations? If you have a close relative with breast cancer or personal history of breast cancer, you may be offered genetic testing for BRCA1/2 mutations.
In women with a BRCA1 or BRCA2 mutation et one additional genetic mutation, or in young women with either a BRCA1 or BRCA2 mutation, a salpingectomy (tube removal) is recommended to reduce the risk of ovarian cancer [7]. The risk of developing ovarian cancer by age 70 if you have BRCA1 is 40-60% (another research study puts the estimates lower, at 39%-46% risk) and 11-27% if you have BRCA2 [7][8].
Should you also have an oophorectomy to reduce ovarian cancer risk if you have BRCA 1 or BRCA2?
Historically, women determined to be at high risk of hereditary ovarian and breast cancer (HBOC) were recommended to undergo preventative removal of both ovaries et both fallopian tubes either a) when the woman had finished childbearing, b) by age 35-40, or c) 10 years before the age of diagnosis of a close relative diagnosed with ovarian cancer. But reality has not matched recommendations, as “it is believed that the majority of these high-risk women do not undergo (risk-reducing salpingo-oophorectomy) by age 40” [7]. This is in part because removal of the ovaries puts young women into surgically-induced menopause, with attendant risks of cardiovascular problems, impaired sexual function, osteoporosis, cognitive impairment, and higher likelihood of death in general.
Fortunately, recent research has allowed the National Comprehensive Cancer Network to more narrowly target its recommendations. Epithelial ovarian cancer is the most common type of ovarian cancer. Researchers now have evidence that the most common and aggressive subtype of epithelial ovarian cancer, high-grade serous carcinoma (as well as, to a lesser extent, epithelial ovarian cancer subtype low-grade serous carcinoma), actually develops in the trompe de Fallope epithelium [7]. Thus, young women with known BRCA mutations may choose to have only their fallopian tubes removed after childbearing is complete, with the potential to remove the ovaries at a later date. The major benefit of this approach is that the young woman does not go into early menopause [7].
Researchers note that removal of the fallopian tubes alone should also reduce risk of epithelial ovarian cancer subtypes clear cell and endometriosis-related ovarian cancer, in addition to the high-grade serous carcinoma and low-grade serous carcinoma subtypes [7].
Salpingectomy to treat tubal ectopic pregnancy
In the case of a tubal ectopic pregnancy (the most common type of grossesse extra-utérine), surgical removal of the entire fallopian tube is sometimes required. This depends on the location of the embryo and/or extent of damage to the fallopian tube [4]. Other times, a salpingostomy (an incision in the tube) can remove the ectopic pregnancy et preserve the fallopian tube for future fertility.
Finally, when a fallopian tube is filled with too much fluid or is severely infected, surgical removal may also be necessary for complete treatment.
How does salpingectomy affect fertility?
While removing the fallopian tubes typically has minimal or no effect on female hormone levels (unlike removing the ovaries), it peut result in reduced fertility (or infertility if both tubes are removed). It’s important to discuss fertility goals, cancer risk, and overall health with a doctor if you’re considering fallopian tube removal.
Tubal ligation
Tubal ligation is a form of permanent contraception, also called female sterilization. It is typically performed laparoscopically, or through an abdominal incision. The fallopian tubes may be cut, tied, clipped, cauterized, or completely removed.
Tubal ligation is not without side effects, some of which (like post-tubal ligation syndrome) can be quite severe, and include painful periods, PMS- and menopause-like symptoms, migraines, and risk of a (non-tubal) ectopic pregnancy (should fertilization still occur). Alternatives like les méthodes de sensibilisation à la fertilité come with none of these side effects, and can be an empowering option for couples seeking to avoid pregnancy indefinitely or permanently.
Le bilan
Understanding the function and health of your fallopian tubes is an integral part of reproductive well-being—even beyond fertilization. Whether or not you’re planning to conceive, being informed about these vital structures can help you make empowered decisions about your health. Blockages or other issues with the fallopian tubes can sometimes lead to chronic pelvic pain, ectopic pregnancies, or infections that may cause complications if left untreated. Being aware of tubal issues can help you advocate for your health and prevent complications.