Some women are relieved to not have a period for the duration of a pregnancy, and for at least the first few months of breastfeeding. But what is not commonly talked about is the four to six weeks of postpartum bleeding and discharge that occurs after birth, otherwise known as lochia.
Lochia looks “bloody” at first, which is why it is sometimes referred to as postpartum bleeding. However, lochia is made up of more than just red blood cells, and it is also not a menstrual bleed—although it certainly seems to make up for the 9 months of not menstruating! So let’s talk about what lochia is, what the first four to six weeks look like for fertility charting postpartum as you wait for lochia to resolve, and when to contact your doctor if your postpartum bleeding seems abnormal.
What is postpartum bleeding, or “lochia,” and how long does it last?
For nine months, give or take, your baby has been living in the womb, swimming around in amniotic fluid. Thanks to high levels of estrogen and progesterone, the endometrium, or the wall of the uterus, has been building up a nice thick layer of blood, placental tissue, endometrial lining, and mucus. So after the baby is born and the placenta is delivered, there is still a heap of tissue, known as lochia, that needs to clear the uterus (regardless of whether you delivered your baby vaginally or via C-section). But unlike the baby and placenta, which come out whole and all at once, this residual tissue is gradually sloughed off over a time period ranging between four to six weeks.
When the placenta detaches from the wall of the endometrium, an open wound (called the placental site) is left, and it can be up to 8.5 inches in diameter. To give you some perspective, that’s the size of a dinner plate. So not only is a new mother going through the bleed of all bleeds during this time, but her body is also working to heal this open lesion in the uterus. This is just another reason why new moms should be doing very little but bonding with their new little one, resting, hydrating, and nourishing their babies—and themselves. When new moms do too much, their flow of lochia often increases in amount as the placental site bleeds, slowing the healing process. When they are able to rest, lochia is often less, and healing can begin much faster. This explains why some women will see their postpartum bleeding stop and start again if they are too active in the early days postpartum.
The 3 stages of Lochia
There are 3 stages of lochia, each one progressing to the next.
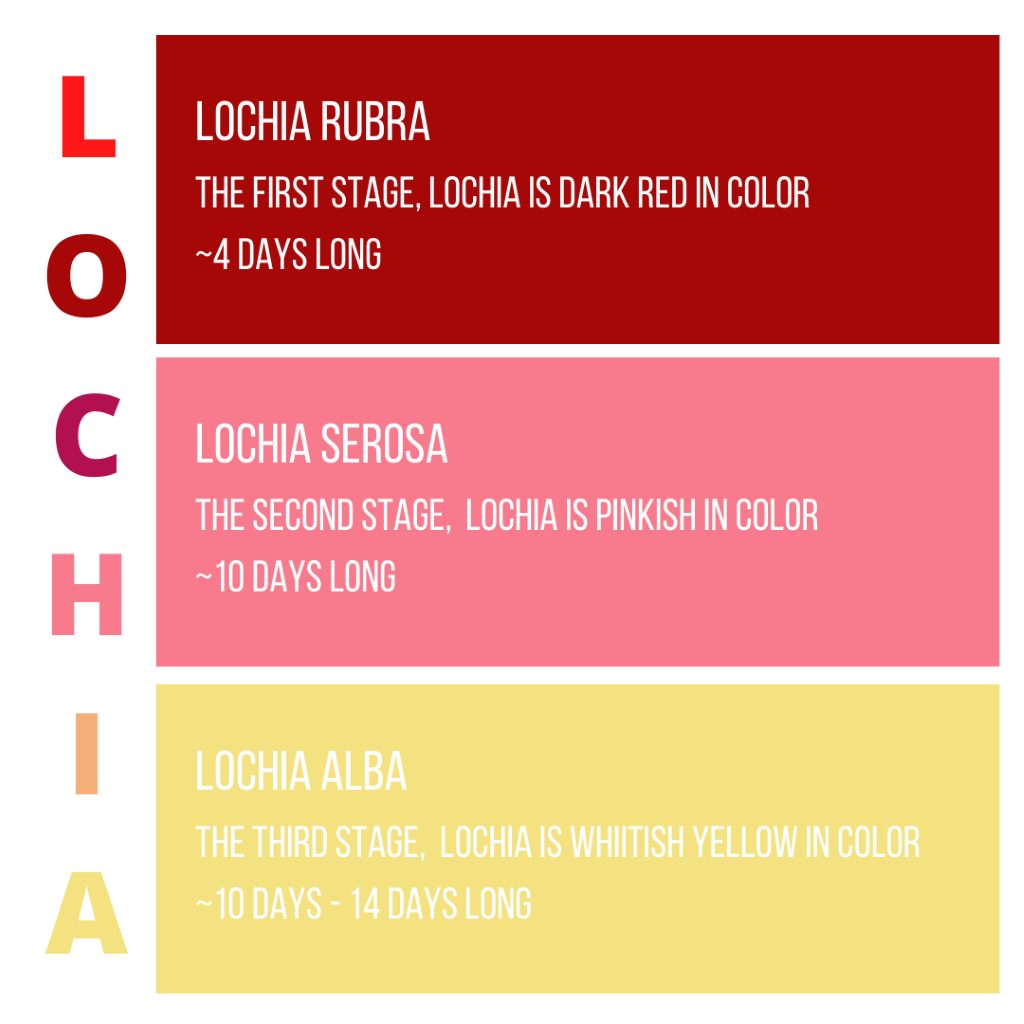
The First Stage: Lochia Rubra
The Rubra stage lasts for about the first four days after you’ve delivered your baby. The first stage is accompanied by the most cramping, since the uterus is still shrinking back to its original, much smaller size. Many breastfeeding women notice that whenever the baby latches on, they almost immediately begin to experience lower abdominal cramping, akin to menstrual cramps. This is due to the oxytocin rush that occurs with suckling and a milk “letdown.”
Many women may also notice a “gush” of blood when they stand up after sitting, due to blood pooling within the vagina. During the Rubra stage, lochia bleeding will be bright red and may have some clots, but these clots shouldn’t be big or difficult to pass. Clots are caused by pooling blood and occur in the first two weeks after giving birth, but not usually after. The rule of thumb is that anything larger than a golf ball warrants a call to your healthcare provider.
The Second Stage: Lochia Serosa
The Serosa stage lasts about 10 days, beginning when postpartum bleeding transitions from bright red to pink, or even to brown. At this point, there are proportionately more white blood cells than red blood cells in the lochia, which is the primary reason for the change in color. During this time, the placental site is still healing, but has made major progress in a short amount of time. Around this point, women may see what they think is fertile cervical fluid. If they are not breastfeeding at all, it certainly could be. However, for women who are breastfeeding, the discharge is more likely to be cells from the cervix continuing to slough off the remains of the mucus plug.
The Third Stage: Lochia Alba
This Alba stage is the final (and longest) stage of postpartum discharge. At this point, it may not even look like bleeding anymore. Lochia will be a yellowish-whitish color, and consists of cervical mucus, white blood cells, and epithelial tissue. The placental site is rapidly creating new skin tissue to heal, which results in more sloughed off tissue.
When it’s all said and done, on average, all three stages of lochia last four to six weeks total. But depending on the new mother’s activity and stress level, it can go longer or shorter.
What does lochia mean for postpartum sex and for fertility charting?
The return to fertility after giving birth is wildly variable depending on a whole host of circumstances. Even for the same woman, the return to fertility can vary after each new baby. But in those first four to six weeks, most moms don’t need to worry about ovulation happening if they are breastfeeding, or even pumping milk or mixed feeding. After those six weeks, it’s a little less certain, depending on how you’re feeding your baby.
If you are more interested in greater certainty of pregnancy prevention, consider charting with a fertility awareness method while breastfeeding. At Natural Womanhood, we have covered this topic in other articles, which can be found here and here. Working with a certified FAM instructor is always highly encouraged to ensure efficacy rates of pregnancy prevention, and especially so during this transitional phase.
Between healing from a vaginal delivery or a C-section, enduring sleepless nights, figuring out feeds, and dealing with a newborn’s general fussiness, fertility charting is usually the last thing a new mom wants to think about. Not to mention that, while there’s no definitive timeline for when a new mom is considered “cleared” for intercourse (the standard answer is about six weeks, but each individual is different and some may need more time), it’s not typically very high on the priority list for new parents. So, as a FAM instructor, I generally tell women not to stress about beginning charting again at any particular time during those first 4 to 6 weeks; you should simply begin charting when you either see cervical fluid after lochia has cleared, or when you find yourself even remotely interested in sex again.
Being physically ready for sex is also different than being emotionally ready. A mom may not feel ready due to how the birth unfolded or the pressures of her new and chaotic life. Rest assured that the six week “clearance” from your doctor may not take into account all of the other variables, like the emotional and psychological ones. Everyone has a different journey. Some women are ready to go at six weeks, while others need more time—even months more time. And that is okay.
Abnormal postpartum bleeding: The warning signs you need to know about
When to contact your care provider:
- If postpartum bleeding doesn’t seem to be getting lighter each day
- If you fill more than one menstrual pad an hour
- If bleeding continues to be bright red and doesn’t transition to brown/pink after the first three days
- If clots are larger than a golf ball
- If blood clots persist past two weeks
- If you have a fever, chills, aches, or a severe headache
- If you have blurred vision, weakness, faintness, or dizziness
- If you experience abdominal pain not related to cramping that accompanies breastfeeding
- If you have foul smelling vaginal discharge (lochia may smell musty, but never foul)
If you experience any of these symptoms, you should immediately contact your OB or midwife. Some of these symptoms may be indicative of postpartum hemorrhage or infection, conditions that can be deadly if not treated promptly. Your care provider will be able to help you navigate which kind of postpartum bleeding is normal and which is not.
Do not be afraid to advocate for yourself during this time—your health and wellbeing is every bit as important as your new baby’s!
When this article refers to fertility awareness methods (FAM), or natural family planning (NFP), we are referring to Fertility Awareness-Based Methods, evidence-based methods of cycle charting which can be used as effective forms of natural birth control when learned by a certified instructor.
Additional Reading:
Three Science-backed, Natural Ways to Ease Childbirth and the Postpartum Period
12 Relatable Instagram Accounts for New Moms to Follow
Can you really use breastfeeding as natural birth control?
Does Breastfeeding Prevent You From Getting Pregnant?
Addressing Our Maternal Mortality Crisis with Fertility Awareness











